Session Information
Date: Sunday, November 13, 2022
Title: Systemic Sclerosis and Related Disorders – Clinical Poster II
Session Type: Poster Session C
Session Time: 1:00PM-3:00PM
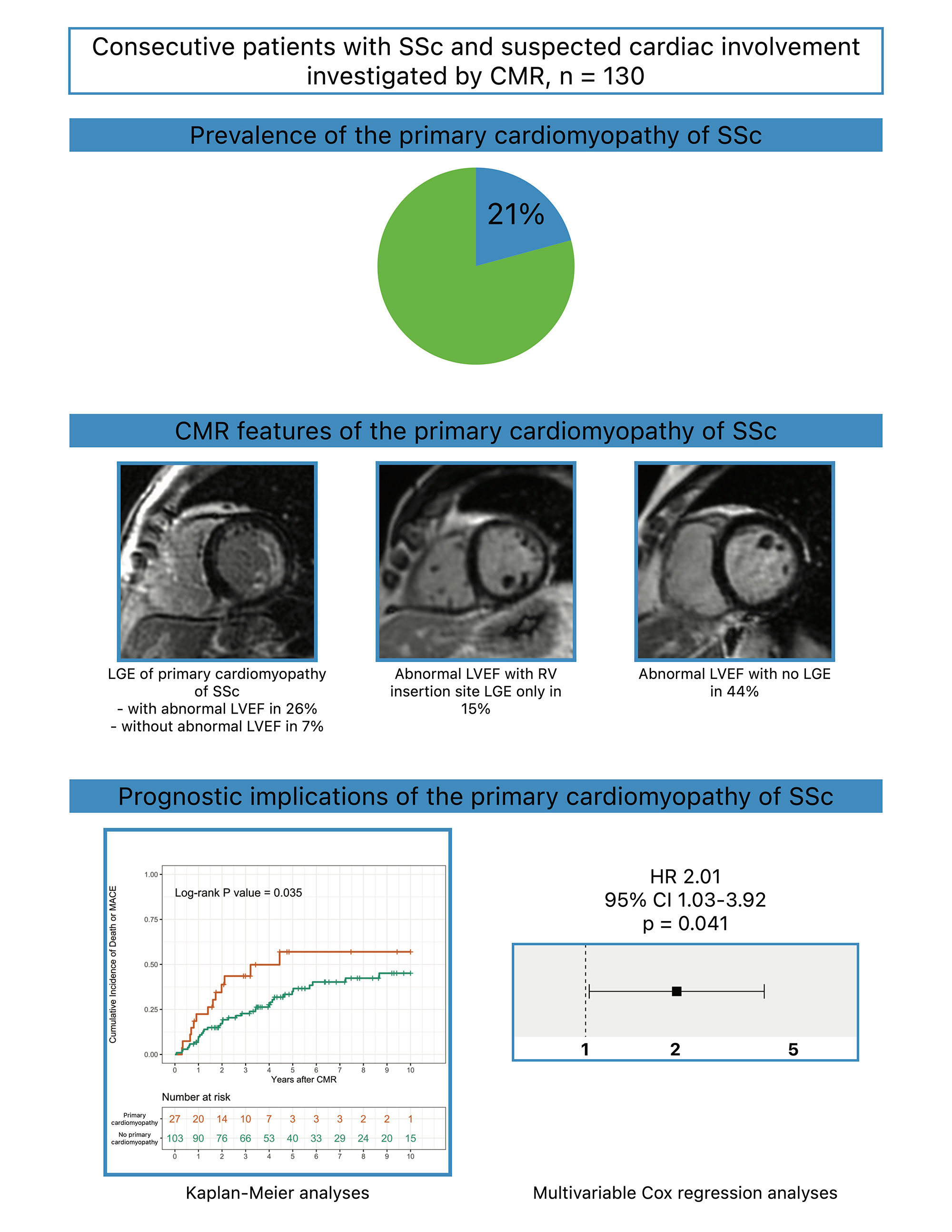
Background/Purpose: Cardiac disease in systemic sclerosis (SSc) may be primary or secondary to coronary artery disease, pulmonary, or renal disease. The prevalence of the primary cardiomyopathy of SSc is unknown. Cardiovascular magnetic resonance imaging (CMR) can help accurately determine the presence of, and the cause of cardiomyopathy. We aimed to study the prevalence, the CMR features, and the prognostic implications of the primary cardiomyopathy of SSc.
Methods: We performed a retrospective cohort study of consecutive patients with SSc meeting the 2013 ACR/EULAR classification criteria who had a clinical CMR for suspected cardiac involvement between 2005 and 2020 at our institution. We defined the primary cardiomyopathy of SSc based on a recent systematic literature review and preliminary data-driven, expert consensus-based definition proposed under the auspices of the World Scleroderma Foundation and the Heart Failure Association of the European Society of Cardiology. We investigated the prevalence and the CMR features of the primary cardiomyopathy of SSc, and its association with the long-term incidence of death or major adverse cardiac events (MACE): heart failure hospitalization, ventricular assist device implantation, heart transplantation, and sustained ventricular tachycardia.
Results: Of 130 patients with SSc who had CMR at a median of 3.6 years after diagnosis, 80% were women, the median age was 58 years, 28% had diffuse cutaneous SSc, 34% had pulmonary arterial hypertension, and 54% had interstitial lung disease. On CMR, 22% had an abnormal left ventricular ejection fraction (LVEF), and 40% had late gadolinium enhancement (LGE). Based on abnormal LVEF and/or LGE not attributable to other causes and/or complications, the prevalence of the primary cardiomyopathy of SSc was 21%. A third of these patients had a distinct LGE phenotype which was widespread subendocardial LVLGE in a pattern that always involved the lateral segments, but in some cases, also extended to other segments, without respecting coronary artery territory distributions, and sometimes also involving the right ventricular aspect of the septum, and the right ventricular free wall. Over a median follow-up of 3.6 years after the CMR, patients with the primary cardiomyopathy of SSc had a greater incidence of death or MACE on Kaplan-Meier analyses (log-rank p=0.035). On multivariable Cox proportional hazards regression analyses, the primary cardiomyopathy of SSc was independently associated with greater long-term death or MACE after adjustment for age, pulmonary hypertension, interstitial lung disease, and renal dysfunction (hazard ratio 2.01; 95% confidence interval 1.03-3.92; p=0.041).
Conclusion: Among consecutive patients with SSc meeting the 2013 ACR/EULAR classification criteria who had clinical CMR for suspected cardiac involvement, the prevalence of the primary cardiomyopathy of SSc was 21%. The primary cardiomyopathy of SSc was independently associated with a greater long-term incidence of death or MACE.
To cite this abstract in AMA style:
Chhikara s, Kanda A, Ismail m, Ogugua F, Rouf R, Ismail k, Bawaskar P, Molitor J, Shenoy C. The Primary Cardiomyopathy of Systemic Sclerosis on Cardiovascular Magnetic Resonance Imaging [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/the-primary-cardiomyopathy-of-systemic-sclerosis-on-cardiovascular-magnetic-resonance-imaging/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-primary-cardiomyopathy-of-systemic-sclerosis-on-cardiovascular-magnetic-resonance-imaging/