Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: High-cost biologic therapies are integral to the management of rheumatoid arthritis (RA), yet access to these agents may be influenced by insurance type, particularly among publicly insured patients who may lack access to copay assistance. This study evaluated whether insurance category is associated with disparities in biologic prescribing patterns and remission outcomes among RA patients.
Methods: A retrospective chart review was conducted of 466 adult RA patients receiving care at a single academic medical center. Patients were stratified into four groups: private insurance, Medicaid, Medicare, and Medicare with supplemental coverage (“Medicare+”). Variables collected included current treatment regimen, route of biologic administration (infusion vs. injectable, including JAK inhibitors), radiographic erosions, seropositivity, demographics, Area Deprivation Index (ADI), Elixhauser Comorbidity Index (ECI), and patient-reported outcomes using the Routine Assessment of Patient Index Data 3 (RAPID3). Multivariable logistic regression analysis was used to assess associations between insurance type and biologic use/remission, adjusting for age, sex, race/ethnicity, and seropositivity.
Results: Biologic use was highest among privately insured patients (52.6%) compared to those with any form of government insurance (45.7%), with the lowest rates observed in Medicare patients (42.5%). Privately insured patients were also more likely to use injectable therapies compared to Medicare and Medicare+ groups (Graph 1). Remission, as assessed by RAPID3, was more common in the privately insured group, with notably lower rates among Medicaid patients (Graph 2). No significant differences were observed across insurance groups in seropositivity, prior treatment history, ECI, or ADI that could account for these disparities (Table 1).
Conclusion: Our project’s findings highlight a 10% disparity in biologic prescribing and patient-reported remission between Medicare and privately insured patients with RA. Moreover, large differences were found in the RAPID3 based on insurance status. While limited by its retrospective, cross-sectional design and single-center sample, this study raises important questions about insurance-related barriers in rheumatologic care. Further research is warranted to explore systemic contributors to treatment inequities and to guide policy aimed at improving equitable access to high-cost therapies.
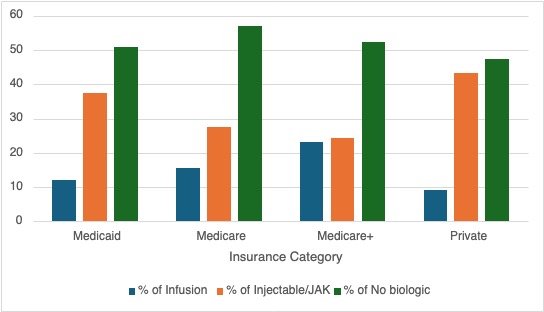 Graph 1: Comparing percentage of Infusion, Injectable/JAK & No Biologic use as a function of Insurance status
Graph 1: Comparing percentage of Infusion, Injectable/JAK & No Biologic use as a function of Insurance status
.jpg) Graph 2: Patient reported outcome (RAPID3) scoring as a function of insurance status
Graph 2: Patient reported outcome (RAPID3) scoring as a function of insurance status
.jpg) Table 1: Comparing patient demographic as a function of insurance status
Table 1: Comparing patient demographic as a function of insurance status
To cite this abstract in AMA style:
Dattagupta A, Diffie C, Cheema S. The Price of Relief: Examining the Role of Insurance in High-Cost Medication Use [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/the-price-of-relief-examining-the-role-of-insurance-in-high-cost-medication-use/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-price-of-relief-examining-the-role-of-insurance-in-high-cost-medication-use/
