Session Information
Session Type: Poster Session D
Session Time: 1:00PM-3:00PM
Background/Purpose: Antibodies to malondialdehyde-acetaldehyde protein adducts (MAA) are increased in both the serum and synovial joint fluid from patients with Rheumatoid Arthritis (RA). These antibodies strongly associate with disease activity and have been demonstrated to predict disease onset. Immunohistochemical (IHC) staining of RA joint tissues for MAA have suggested that extracellular matrix proteins (ECM) are involved in the disease pathogenesis. However, these studies only examined the associations of MAA and ECM proteins to co-localize together in the same area of the joint. Therefore, it was the purpose of this study to determine whether RA patients develop antibodies to MAA modified ECM proteins in the serum and synovial fluid.
Methods: ELISA plates were coated with MAA modified collagen II, vimentin, fibrinogen and incubated overnight at 4oC degrees. Matched serum and synovial fluid from RA patients and OA controls were incubated with the antigen coated plates. Secondary antibodies specific to human IgG, IgM and IgA were added to determine isotype involvement. Detection was accomplished using horseradish peroxidase (HRP) labeled goat anti-human IgG, IgM, or IgA antibodies. Absorbance was determined at 450 nm using an Epoch Plate reader (BioTek) and analyzed using Gene 5 Software (BioTek). Data are expressed in arbitrary units (AU) of MAA antibody relative to the standard curve.
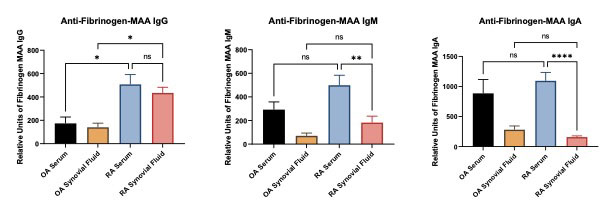
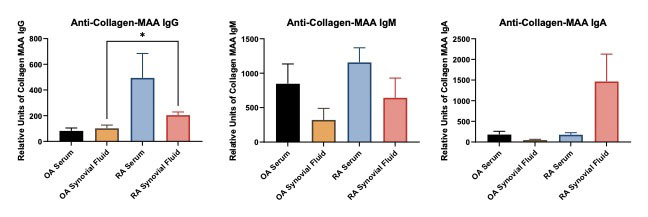
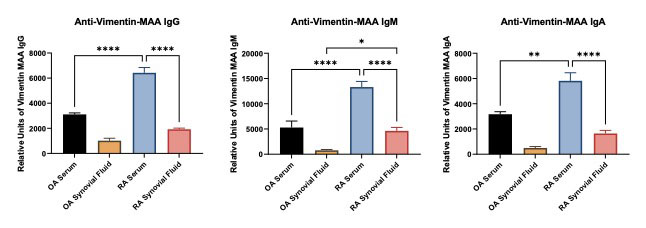
Results: Circulating serum IgG antibodies to MAA adducted ECM proteins were significantly increased in the RA patients compared to OA, CII p< 0.05, VIM p< 0.0001, FIB p< 0.0001. Similar results were observed in the RA synovial fluid compared to the OA, CII p< 0.05, VIM p< 0.0001, FIB p< 0.05. IgM antibodies to ECM proteins in the RA patients demonstrated a significant increase in CII p=NS, VIM p< 0.001, FIB p< 0.01 for both serum and synovial fluid compared to the OA. However, IgA antibodies to ECM proteins showed a unique profile. RA synovial fluid had higher antibodies in CII p< 0.01 compared to serum for both RA and OA patients. Antibodies to FIB were significantly p< 0.01 decreased in the RA synovial fluid compared to OA. Yet, antibodies to VIM were both increased in the serum (p< 0.05) and synovial fluid (P< 0.01) in the RA samples compared to OA. Importantly, vimentin MAA demonstrated the highest antibody concentration for all of the ECM proteins evaluated.
Conclusion: Identification of serum antibodies to MAA modified ECM proteins in the synovial fluid and serum of RA patients provides new insight into the onset or progression of RA. These modified proteins and antibodies to them may be potential biomarkers for the diagnosis/treatment of patients with RA. Further work is needed to elucidate the role these modified proteins are playing in the manifestation of this disease.
To cite this abstract in AMA style:
Taylor A, Duryee M, Hunter C, Aripova n, Mikuls T, Thiele G. The Presence of Anti-MAA Antibodies to Extracellular Matrix Proteins in Synovial Fluid and Sera of Patients with Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/the-presence-of-anti-maa-antibodies-to-extracellular-matrix-proteins-in-synovial-fluid-and-sera-of-patients-with-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-presence-of-anti-maa-antibodies-to-extracellular-matrix-proteins-in-synovial-fluid-and-sera-of-patients-with-rheumatoid-arthritis/