Session Information
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose:
A subset of patients with idiopathic inflammatory myopathy develop significant restrictive lung disease, although risk factors for this are poorly defined. Autoantibodies may be important in defining risk. The primary purpose of this study is to identify clinical and serologic risk factors for development of significant restrictive pulmonary defects on pulmonary function testing in patients with idiopathic inflammatory myopathy.
Methods:
We conducted a retrospective chart review of patients with diagnoses of dermatomyositis, polymyositis, and/or anti-synthetase syndrome with at least one pulmonary function test seen at Rush University Medical Center between January 1, 2010, and October 6th, 2019. We used ICD-9 and ICD-10 codes to identify study patients and confirmed the diagnoses via chart review. We extracted baseline demographic data, relevant disease features, smoking history, serologic data (hemoglobin, muscle enzymes, autoantibody profiles), chest CT reports, and pulmonary function data from the medical record. We compared patients with forced vital capacity (FVC) % predicted < 70 at any time during their clinical course to patients with FVC % predicted ≥ 70, using this cut point to define a significant restrictive defect. We used two-tailed Student’s T-tests to compare continuous variables and Chi square tests (or Fisher’s exact tests) for categorical variables. We used the exploratory analyses to select factors to include in a multivariable logistic regression to model the outcome of FVC% predicted < 70.
Results:
Eighty-eight patients met the inclusion/exclusion criteria. Of these, 50/88 (56.8%) patients had FVC% predicted ≥ 70 and 38/88 (43.2%) patients had FVC% predicted < 70. Patients’ ages ranged from 28.0 to 56.7 years, 48/85 (56.5%) were African-American, and 45/88 (51.1%) had a primary diagnosis of dermatomyositis. Patients with FVC% predicted < 70 had a greater mean CK (4264.3 units/L vs. 1461.0 units/L; p= 0.0412) and were more likely to be positive for anti-Jo1 (4/35 [32.4%] vs. 4/35 [11.4%]; p=0.044), anti-MDA5 (7/17 [41.2%] vs. 3/19 [15.8%]; p=0.139), and anti-PL7 (4/17 [23.5%] vs. 1/20 [5.0%]; p= 0.159) antibodies. Multivariable logistic regression demonstrated that the presence of anti-Jo-1, anti-MDA5, and/or anti-PL-7 antibodies was independently associated with a significant restrictive pulmonary defect (OR 18.49 95% CI 2.13-160.76; p = 0.008).
Conclusion:
The presence of anti-PL-7, anti-Jo1, and/or anti-MDA5 antibodies was associated with a nearly 19-fold increased risk of significant restrictive pulmonary defect in this cohort of patients with dermatomyositis and polymyositis. Patients with a significant restrictive defect had greater mean CK levels, but CK level was not an independent risk factor for a significant restrictive defect in multivariable analyses. Future studies should be conducted to validate these findings in an external cohort and to differentiate between restrictive pathology due to ILD and restrictive pathology due to muscle weakness.
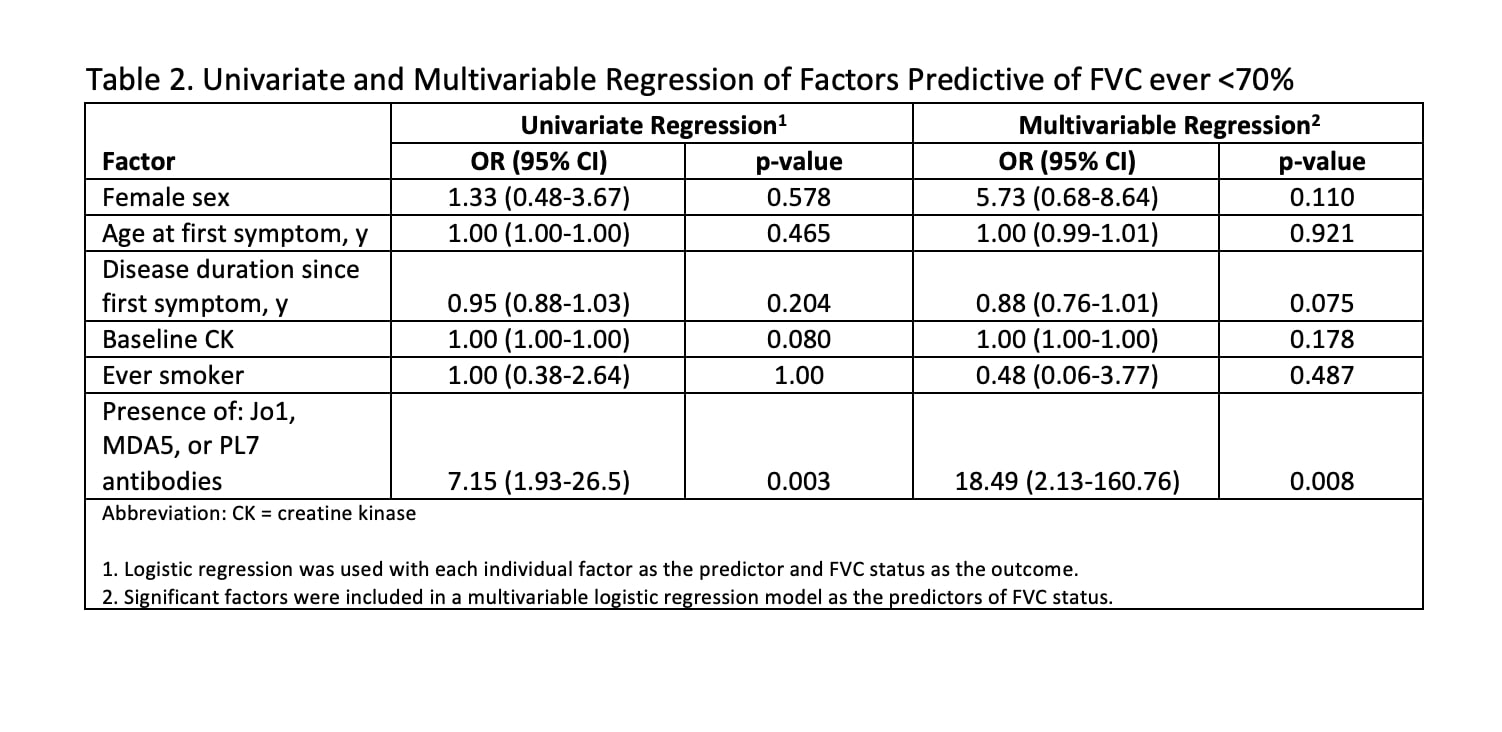 Univariate and Multivariable Regression of Factors Predictive of FVC Ever < 70%
Univariate and Multivariable Regression of Factors Predictive of FVC Ever < 70%
To cite this abstract in AMA style:
Cherny D, Richardson C. The Presence of Anti-Jo1, anti-PL7, And/or anti-MDA5 Antibodies in Idiopathic Inflammatory Myopathy Confers an Increased Risk of a Significant Restrictive Pulmonary Defect [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/the-presence-of-anti-jo1-anti-pl7-and-or-anti-mda5-antibodies-in-idiopathic-inflammatory-myopathy-confers-an-increased-risk-of-a-significant-restrictive-pulmonary-defect/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-presence-of-anti-jo1-anti-pl7-and-or-anti-mda5-antibodies-in-idiopathic-inflammatory-myopathy-confers-an-increased-risk-of-a-significant-restrictive-pulmonary-defect/
