Session Information
Date: Monday, October 27, 2025
Session Type: Abstract Session
Session Time: 4:00PM-4:15PM
Background/Purpose: Perimenopause is associated with a wide spectrum of symptoms, including mood changes, sleep disturbances, and joint pains. Limited information exists on the effect of perimenopause on psoriatic arthritis (PsA). We assessed whether PsA disease activity worsens during perimenopause compared to the pre- and post-menopause stages.
Methods: We analyzed data on female patients with PsA followed in a prospective cohort from 1978 to 2024. Data on PsA disease activity, medications, co-morbidities, and age at menopause were collected using standard protocols. Pre-perimenopausal and post-menopausal stages were defined as >2 years before and after the final menstrual period (FMP), respectively, while the perimenopause stage was within two years (before or after) of the FMP. PsA disease activity was assessed at each visit using Disease Activity in PsA (DAPSA), tender and swollen joint counts, PASI, CRP, and FACIT-fatigue. Disease activity during the perimenopause stage was compared to the pre-perimenopause and post-menopause visits. The association between menopausal stages and PsA disease activity measures was assessed with a Generalized Additive Model with splines (considering time from FMP as continuous variable) and with linear mixed-effects models (considering menopausal stages as categorical variables). Each model was adjusted for age, disease duration, and medication use, and accounted for repeated observations via a subject-specific random effect. We assessed the mediating effects of BMI and fatigue on the increase in DAPSA during perimenopause.
Results: A total of 477 female patients provided data for 8,381 visits over a mean follow-up of 12.1 years. Mean age at first visit was 44.9±13.9 years, and mean age at menopause was 48.7 years. Hormone replacement therapy had been used by only 1.5% of patients at any time point. A rise in DAPSA scores was found during perimenopause years, followed by a slight drop post-menopause (Figure 1). Linear mixed models found an association between being in perimenopause and higher DAPSA compared to the pre-perimenopause (β = 1.92, p< 0.001) and post-menopause stages (β = 1.56, p=0.001, Table 1). Significantly higher tender and swollen joint counts were found in perimenopause compared to both pre- and post-menopause. Higher PASI scores were found in perimenopause compared to the post-menopause stage (Table 1). An increase in fatigue levels during perimenopause only partially mediated the increase in DAPSA during perimenopause, explaining 12% to 18% of this change (Figure 2). BMI did not have a mediating effect on DAPSA change during perimenopause.
Conclusion: Perimenopause is associated with an increase in PsA disease activity, which includes both patient-reported outcomes and objective measures of activity. These findings highlight the need to study the effect of hormone replacement therapy in perimenopausal PsA patients.
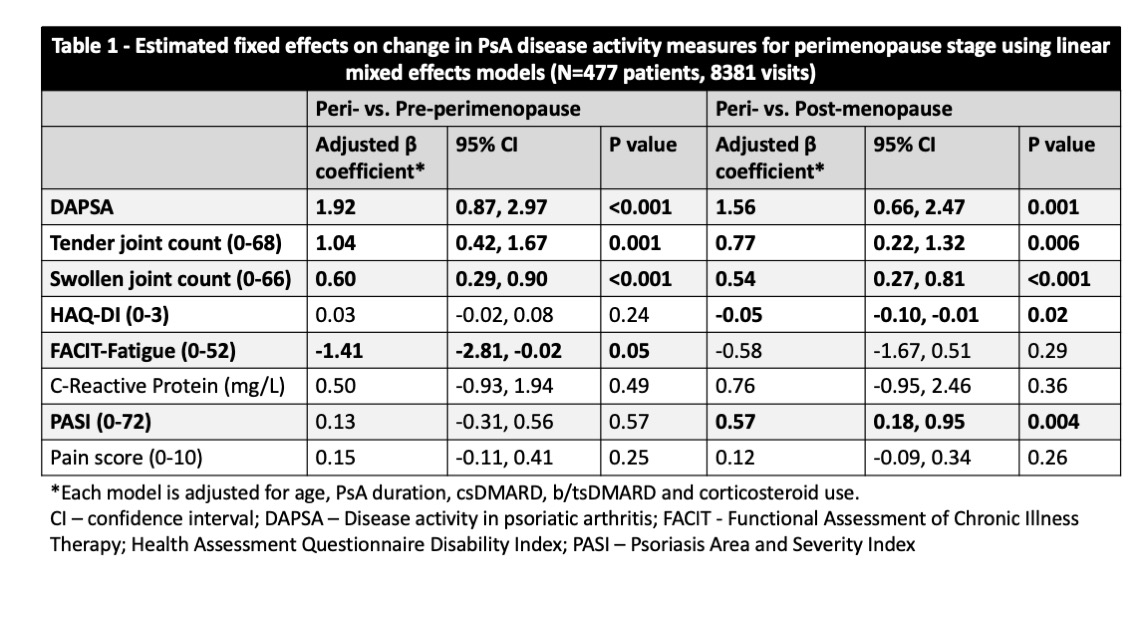 Figure 1: Time from final menstrual period (FMP) estimated partial effect on the individual mean DAPSA score by Generalized Additive Model adjusted for age, disease duration and medication use
Figure 1: Time from final menstrual period (FMP) estimated partial effect on the individual mean DAPSA score by Generalized Additive Model adjusted for age, disease duration and medication use
.jpg) Table 1 – Estimated fixed effects on change in PsA disease activity measures for perimenopause stage using linear mixed effects models
Table 1 – Estimated fixed effects on change in PsA disease activity measures for perimenopause stage using linear mixed effects models
.jpg) Figure 2: Assessment of the mediating effect of BMI and fatigue on DAPSA change during peri-menopause.
Figure 2: Assessment of the mediating effect of BMI and fatigue on DAPSA change during peri-menopause.
To cite this abstract in AMA style:
Eder L, Li X, Koppikar S, Lega I, Gladman D, Chandran V, Cook R. The perimenopause period is associated with increased levels of disease activity in psoriatic arthritis [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/the-perimenopause-period-is-associated-with-increased-levels-of-disease-activity-in-psoriatic-arthritis/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-perimenopause-period-is-associated-with-increased-levels-of-disease-activity-in-psoriatic-arthritis/
