Session Information
Date: Sunday, October 26, 2025
Title: (0430–0469) Rheumatoid Arthritis – Diagnosis, Manifestations, and Outcomes Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: RA-related pain is typically thought of as pain in the joints. However, non-articular pain (NAP) is also common, persisting in 1/3 of patients with early RA despite treatment (1). NAP may prevent patients from achieving treatment goals by contributing to elevated pain intensity and patient global assessment (PtGA). Overestimation of disease activity may lead to changes in DMARD treatment without associated improvements in disease outcomes. Recognizing NAP as a driver of pain intensity and PtGA may help prevent overtreatment with DMARDs, lead to earlier recognition of and addressing treatment with greater specificity for different types of pain. Our aims were to evaluate the cross-sectional association of NAP with elevated pain intensity and PtGA in patients 3-months after initiating a new DMARD for active RA.
Methods: The Central Pain in Rheumatoid Arthritis study is a prospective cohort of patients fulfilling 2010 ACR/EULAR criteria for RA, who have active disease and are initiating a new DMARD. At the 3-month visit, patients indicated any areas of pain or tenderness that they were experiencing on a body pain diagram (BPD), derived from the Widespread Pain Index which assesses 19 body areas (jaw, neck, shoulder (girdle), upper arm, lower arm, upper back, chest, abdomen, lower back, hip (buttock), upper leg and lower leg). Prespecified NAP patterns were classified based on pain reported in 5 sections (4 quadrants and axial, excluding hands and feet) and grouped as: 1) no NAP (no sections selected), 2) regional (1-3 sections) or 3) widespread NAP (4-5 sections) (1). Patients completed synchronous assessments of pain intensity and PtGA. Separate median regression models were used to examine the associations between NAP groups and the two outcomes. Both unadjusted and adjusted models (controlling for age, sex, education, smoking status, comorbidity, seropositivity, and study site) were fitted.
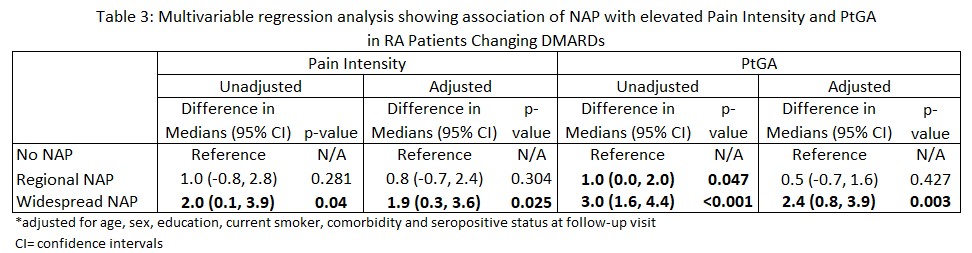
Results: The 192 RA patients were mostly female (84%) with mean (SD) age of 55 (14) years; 70% were seropositive, mean RA disease duration was 10.8 (212.8) years and mean (SD) CDAI was 14.9 (12.6) (Table 1). NAP was prevalent in 92.7% (n=178), with regional NAP 44.3% (n=85) and widespread NAP 48.4% (n=93). Compared to other groups, those with widespread NAP were more frequently White women who reported more comorbidities and longer disease duration. At follow-up, NAP was associated with higher median values [IQR] for pain intensity and for PtGA in a dose-dependent fashion across pain groups: no NAP, regional NAP and widespread NAP (Table 2). In median regression analyses, compared to no NAP, widespread NAP was associated with higher median levels of both pain intensity and PtGA: difference in medians 95%[CI] was 1.9 (0.3, 3.6) and 2.4 [0.8, 3.9], respectively (Table 3).
Conclusion: NAP was associated with higher pain intensity and PtGA in RA in a dose-dependent fashion. Despite changing DMARD treatment to manage active RA, widespread NAP was identified as a significant driver of pain intensity and PtGA. A limitation includes a lack of validated tool to screen for NAP in RA, calling for improved reporting of NAP. Early identification and intervention of NAP may help patients to reach their treatment goals.1. Meng et al. doi: 10.1002/art.43049.
To cite this abstract in AMA style:
Meng C, Song J, muhammad L, Julia C, Neogi T, Bolster M, Marder W, Bingham C, Lee Y. The Painful Truth: Non-Articular Pain’s Impact on Rheumatoid Arthritis Assessment after Initiating a new DMARD for Active Disease [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/the-painful-truth-non-articular-pains-impact-on-rheumatoid-arthritis-assessment-after-initiating-a-new-dmard-for-active-disease/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-painful-truth-non-articular-pains-impact-on-rheumatoid-arthritis-assessment-after-initiating-a-new-dmard-for-active-disease/

.jpg)
.jpg)