Session Information
Session Type: Poster Session B
Session Time: 5:00PM-6:00PM
Background/Purpose: Juvenile Dermatomyositis (JDM) is theorized to occur in a genetically susceptible individual as a response to an environmental trigger, leading to autoimmunity and inflammation. Several viruses have been linked to the underlying pathophysiology of JDM, with few reports of SARS-CoV-2 infection associated with both initial episodes and flares of JDM around the world. In this study, we sought to investigate the impact of the COVID-19 pandemic on our population of JDM patients and evaluate the number of new JDM diagnoses and JDM flares during the pandemic, as compared to 5 years pre-pandemic.
Methods: Biomedical Informatics identified patients 21 years and younger using the ICD-10 code M33, who were diagnosed between June 2015 and December 2022. Data were collected retrospectively comparing manifestations of JDM patients initial presentations and flares pre-pandemic (6/1/15-2/28/20) as well as during the pandemic (3/1/20-12/30/22). Information about known COVID-19 exposures and infections preceding a flare or initial diagnosis was assessed. Flare episodes were characterized by clinical symptoms, physical exam findings, pertinent labs, and medications at the time of flare. Exploratory data analysis was used to explore potential relationships between flares occurring before and during the pandemic using summary statistics, univariate and bivariate analysis.
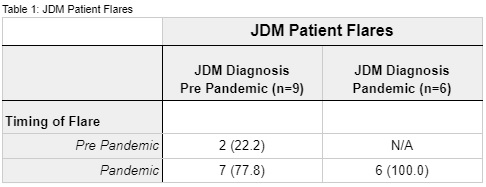
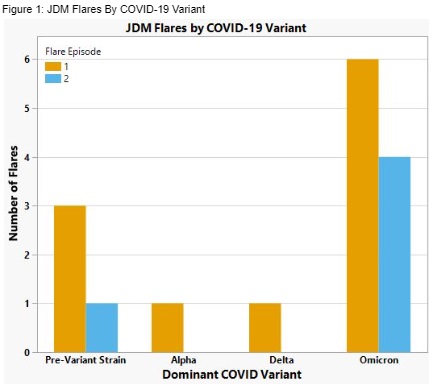
Results: Seventeen patients diagnosed with JDM were identified; 8 pre-pandemic and 9 during the pandemic. Fifteen flares were captured from 12 patients, of which 87% (13/15) occurred during the pandemic (Table 1). Of those JDM patients diagnosed pre-pandemic, 78% of their flares occurred during the pandemic. Of the 12 patients who experienced flares, 80% of these patients experienced at least one flare, while 25% experienced more than one flare during the pandemic. Fifteen percent of patients who experienced flare had a medication (Methotrexate) held for COVID-19 vaccination; 55% of our patients were vaccinated. Two patients had documented COVID-19 infections preceding flare. The majority of flares occurred during the time period when Omicron variants of COVID-19 were predominant (12/1/21 to 12/30/2022) (Figure 1).
Conclusion: The majority of flares in this study period occurred during the pandemic. Although a minority of patients had documented COVID-19 infection preceding flare, most flares occurred during the time when Omicron variants were predominant; therefore, these patients may have had undocumented or asymptomatic COVID-19 infections that potentially triggered flares. Holding immunomodulating medications to optimize immune response to COVID-19 vaccination may have also potentially contributed to flares. An increase in telehealth visits during the pandemic may have also led to suboptimal monitoring and disease control in JDM potentially modulating the number of JDM flares during the pandemic. Future investigation of the COVID-19s impact in larger cohorts would elucidate correlations between the pandemic, COVID-19 infections, and vaccinations with JDM flares.
To cite this abstract in AMA style:
Ambooken T, Kadakia S, Lozy T, Bulbin B, Ganguli S, Wahezi D, Lapidus S. The Impact of the COVID-19 Pandemic on Juvenile Dermatomyositis [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 4). https://acrabstracts.org/abstract/the-impact-of-the-covid-19-pandemic-on-juvenile-dermatomyositis/. Accessed .« Back to 2023 Pediatric Rheumatology Symposium
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-impact-of-the-covid-19-pandemic-on-juvenile-dermatomyositis/