Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Previous literature has suggested racial and ethnic variations in the clinical expression of psoriatic disease, with Non-White patients having more extensive skin disease, higher disease activity, frequent axial involvement and more comorbid disease1-3. Additionally, ethnic minority psoriatic arthritis (PsA) patients have delays in diagnosis and less use of biologic medications.2,4. Data on potential confounders, such as socioeconomic variables, particularly neighborhood social deprivation defined by prior redlining policies, are limited. Historically, majority Black neighborhoods were considered high risk for investment (redlined), limiting opportunities for Black homeownership and stunting neighborhood development5. We aimed to evaluate the association of neighborhood social deprivation and disease burden amongst racial and ethnic subsets of PsA patients.
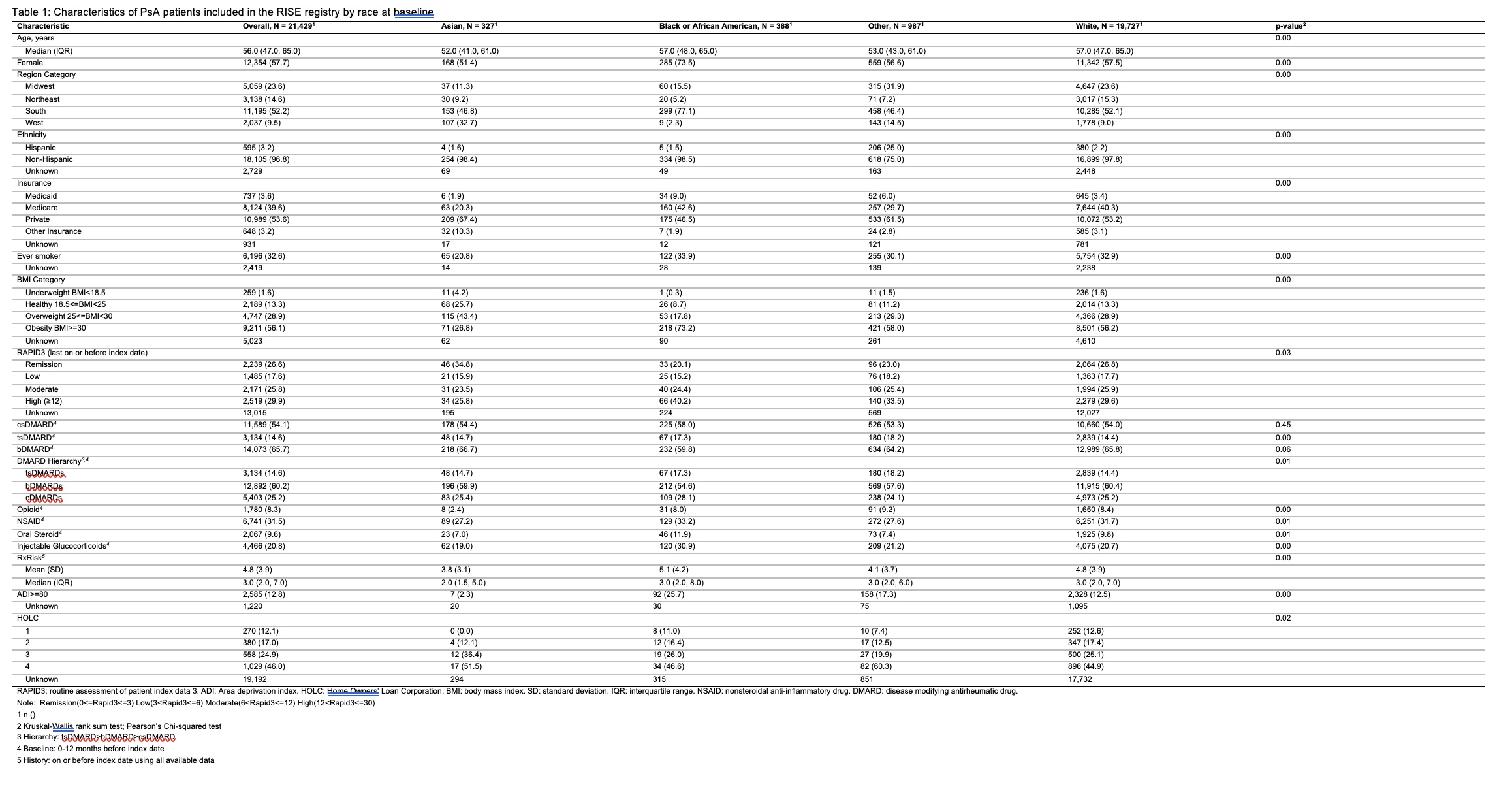
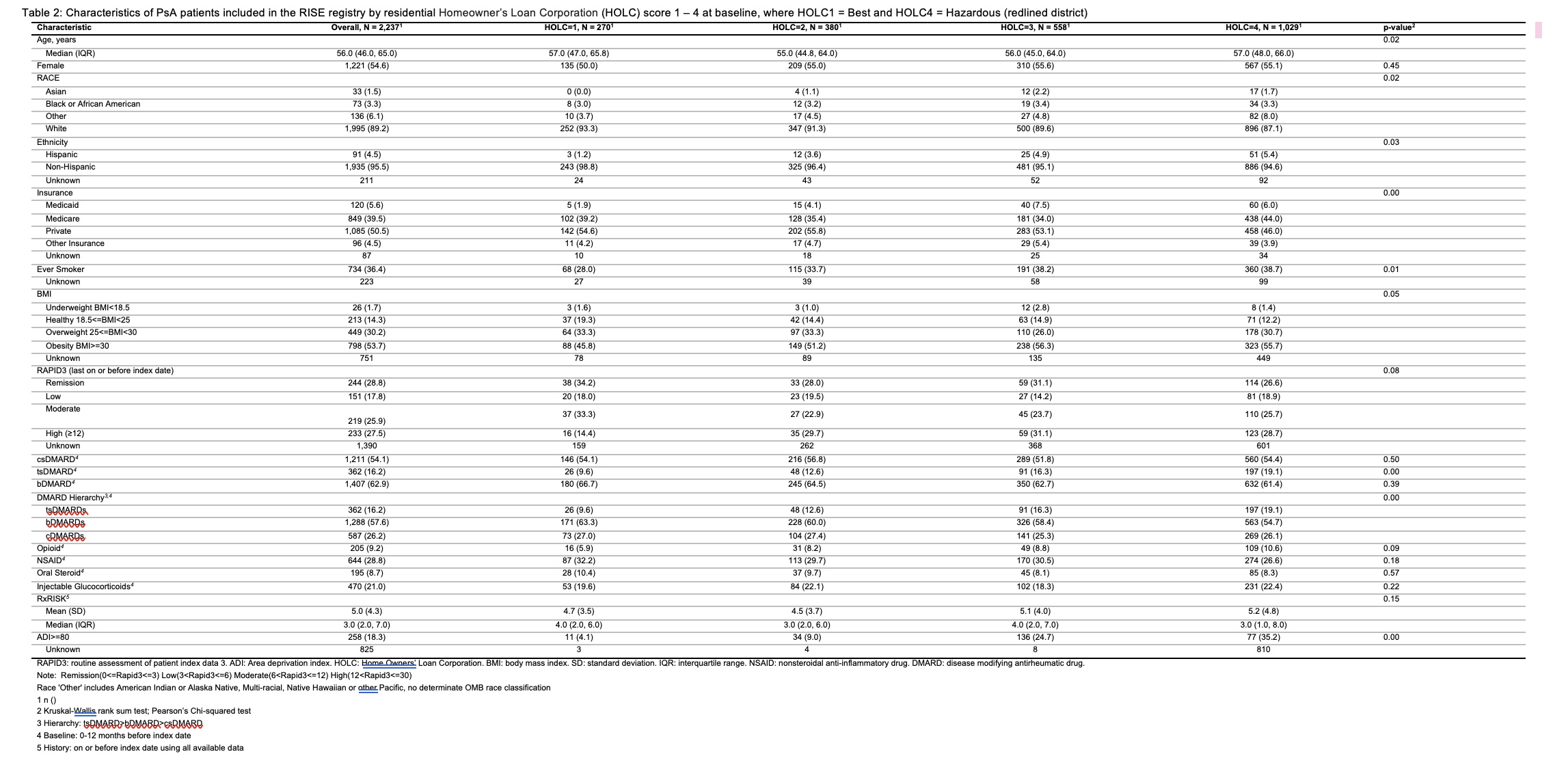
Methods: Our PsA cohort included patients with ≥2 diagnoses of PsA defined by ICD 9/10 codes enrolled in the ACR Rheumatology Informatics System for Effectiveness (RISE) registry with self-reported race, geographic region of residence and at least 3 years of follow-up. We examined the distribution of demographics, disease activity, including high disease activity (HDA: RAPID3 >12), social deprivation (Area Deprivation Index [ADI, high ≥ 80), and treatments overall, and stratified by race. We conducted a subgroup analysis assessing demographic and clinical characteristics of PsA patients stratified by historical residential security grades [Home Owner’s Loan Corporation – HOLC1 (‘best’ residence location) to HOLC4 (‘hazardous’ residence location = historically redlined district)].
Results: The study cohort included 21,429 PsA patients. Patients had median age 55 (12.8) years and were predominantly female (57.7%), obese (56.1% BMI >30), and residing in the South (52.2%) (Table 1). ADI ≥ 80th percentile (high deprivation) was greatest among Black patients (25.7 % vs. 2.3% Asian, 17.3% Other, and 12.5% White), who also had the greatest proportion of HDA (40.2% vs. 25.8% Asian, 29.6% White, and 33.5% Other). Approximately 5% of PsA patients lived in historically redlined districts, which consisted of mostly Black and Other non-White patients (8.8% and 8.3%, respectively). Of the 2,237 PsA patients residing in areas with a defined HOLC score (Table 2), there was greater prevalence of Hispanic and Other compared to White patients in HOLC4 vs HOLC1. Smoking, obesity, ADI ≥ 80th percentile, federal insurance and HDA were also more prevalent in historically redlined areas. HOLC4 patients also spent more time in HDA (median 81.5 person days [IQR 0, 651]) and less time in remission (median 0 person days [0, 542]), and had a greater proportion of targeted synthetic DMARD use [19.1% vs HOLC1 9.6%], and a somewhat lower proportion of biologic DMARD use (61.4% vs. HOLC1 66.7%).
Conclusion: In the US, disparities exist for Black patients with PsA, who have more prevalent high disease activity and high social deprivation. In addition, the enduring effects of structural racism appear to negatively influence the disease characteristics of PsA in patients living in historically redlined areas.
To cite this abstract in AMA style:
Banbury B, Dowell S, Jenkins C, Holladay E, Xie F, Zhang J, Wright G, Curtis J, Kerr G. The Impact of Race and Ethnicity and Historical Redlining on Psoriatic Disease Burden [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/the-impact-of-race-and-ethnicity-and-historical-redlining-on-psoriatic-disease-burden/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-impact-of-race-and-ethnicity-and-historical-redlining-on-psoriatic-disease-burden/