Session Information
Session Type: Poster Session B
Session Time: 9:00AM-10:30AM
Background/Purpose: To examine the association between antimalarial (AM) adherence and acute care utilization among newly diagnosed rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE) patients.
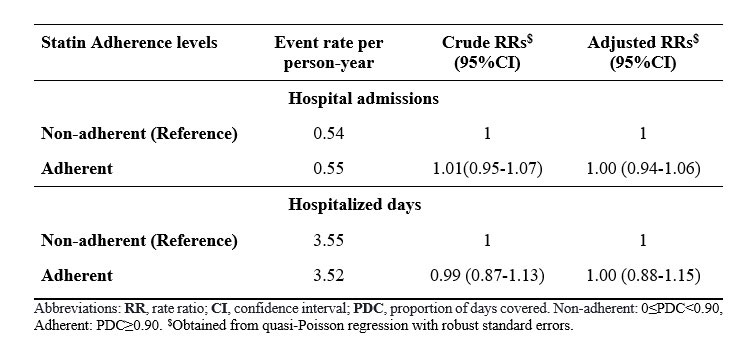
Methods: We used administrative databases for British Columbia, Canada, to conduct a population-based propensity score (PS) matched study of incident cohorts of RA and SLE with incident AM use between January 1997 and March 2014. Index date was defined as the time when subjects met RA/SLE criteria and had AM. Only subjects with at least one year of follow-up were retained. In the first year (“baseline year”), we calculated AM adherence using proportion of days covered (PDC) and categorized as adherent (PDC≥0.90) or non-adherent (0≤PDC< 0.90). We computed a PS for AM adherence using baseline variables on demographics, comorbidities, other medications, and healthcare utilization evaluated over 12 months prior to index date; RA or SLE disease duration, and prior AM use duration at index date. Each AM adherent patient was matched with up to two AM non-adherent patients. Our outcomes include the number of hospital admissions and hospitalized days assessed in the following year (“follow-up year”). We used quasi-Poisson regression models with robust standard errors to examine the impact of AM adherence during the baseline year on these two outcomes in the follow-up year, adjusting for above baseline variables in the matched sample. Using the same design, we examined the association between acute care utilization and the adherence of an unrelated drug, statin, as a falsification test to rule out the possibility of confounding by unmeasured healthy adherer effect: one expects to find no association if the study design adequately controls for potential healthy adherer bias since statin adherence is not expected to have immediate effect on acute care utilization.
Results: We identified 5,997 AM adherent and 13,841 AM non-adherent incident RA and SLE patients. After PS matching, 5,996 AM adherent (mean age 58.9 years, 74.3% female) and 11,241 matched AM non-adherent (mean age 57.8 years, 75.1% were women) were included in the analysis (total = 17,237). After matching, all baseline variables between AM adherent and non-adherent patients were well balanced, with all standardized differences less than 0.10 (Table 1). The crude rates for hospital admissions were 0.39 and 0.42 per person-year for adherent and non-adherent patients in the follow-up year, respectively. The respective crude rates for hospitalized days were 2.18 and 2.66 per person-year. Using the quasi-Poisson models, the adjusted rate ratios (RRs) of hospital admissions and hospitalized days obtained for AM adherent vs. non-adherent patients were 0.88 (95% CI: 0.83-0.94) and 0.78 (95% CI: 0.68-0.90), respectively (Table 2). The falsification test showed that our matched study design is unlikely to be subject to unmeasured healthy adherer effect (Table 3) since a protective association was not found for statin adherence.
Conclusion: Adherence to AM therapy in RA and SLE patients was associated with a lower risk of future acute care utilization (12% reduction in the risk of hospital admission and 22% reduction in the number of hospitalized days) compared to patients with non-adherence.
To cite this abstract in AMA style:
Hoque M, Avina-Zubieta J, Lacaille D, De Vera M, Qian Y, Esdaile J, Xie H. The Impact of Early Antimalarial Adherence on Future Acute Care Utilization Among Rheumatoid Arthritis and Systemic Lupus Erythematosus Patients: A Population-based Study [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/the-impact-of-early-antimalarial-adherence-on-future-acute-care-utilization-among-rheumatoid-arthritis-and-systemic-lupus-erythematosus-patients-a-population-based-study/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-impact-of-early-antimalarial-adherence-on-future-acute-care-utilization-among-rheumatoid-arthritis-and-systemic-lupus-erythematosus-patients-a-population-based-study/