Session Information
Session Type: Poster Session B
Session Time: 9:00AM-10:30AM
Background/Purpose: Hip and knee total joint arthroplasties (TJA) for osteoarthritis (OA) are frequently performed surgical procedures, representing the majority of direct expenditures for OA. TJA demand is expected to continue increasing with the aging population. Despite their relatively high effectiveness, as many as 20% of patients continue to report residual symptoms post-TJA. Comorbid diabetes is common in OA. While diabetes is associated with higher rates of post-TJA complications (e.g. infection), few studies have examined diabetes impact on TJA patient-reported outcomes, with variable findings. Given known sex and body mass index (BMI) differences in OA, TJA and diabetes, we investigated the association between diabetes and post-TJA disability and pain, explicitly examining whether diabetes impact may differ by sex and BMI.
Methods: Patient sample underwent primary hip or knee TJA for OA from Nov 2015 to Dec 2018. All patients provided written informed consent. Eligibility criteria: ≥35 years of age and English fluency. Exclusion criteria: acute trauma/injury, inflammatory arthritis, revision surgery. Patient height and weight were measured pre-surgery. Pre-surgery, patients completed questionnaires capturing data on sociodemographic characteristics, comorbidity, symptomatic joints, opioid use and symptoms of depression and anxiety (HADS), and neuropathic pain (painDETECT). Hip/knee pain and disability (WOMAC) were captured pre- and 1-year post-surgery. Patient-reported ‘non-response’ was defined as < 30% improvement in 1) WOMAC pain and 2) WOMAC disability, at 1-year relative to pre-surgery. A series of adjusted logistic regression models (outcome: response no vs. yes) were estimated testing interactions between diabetes, sex and BMI.
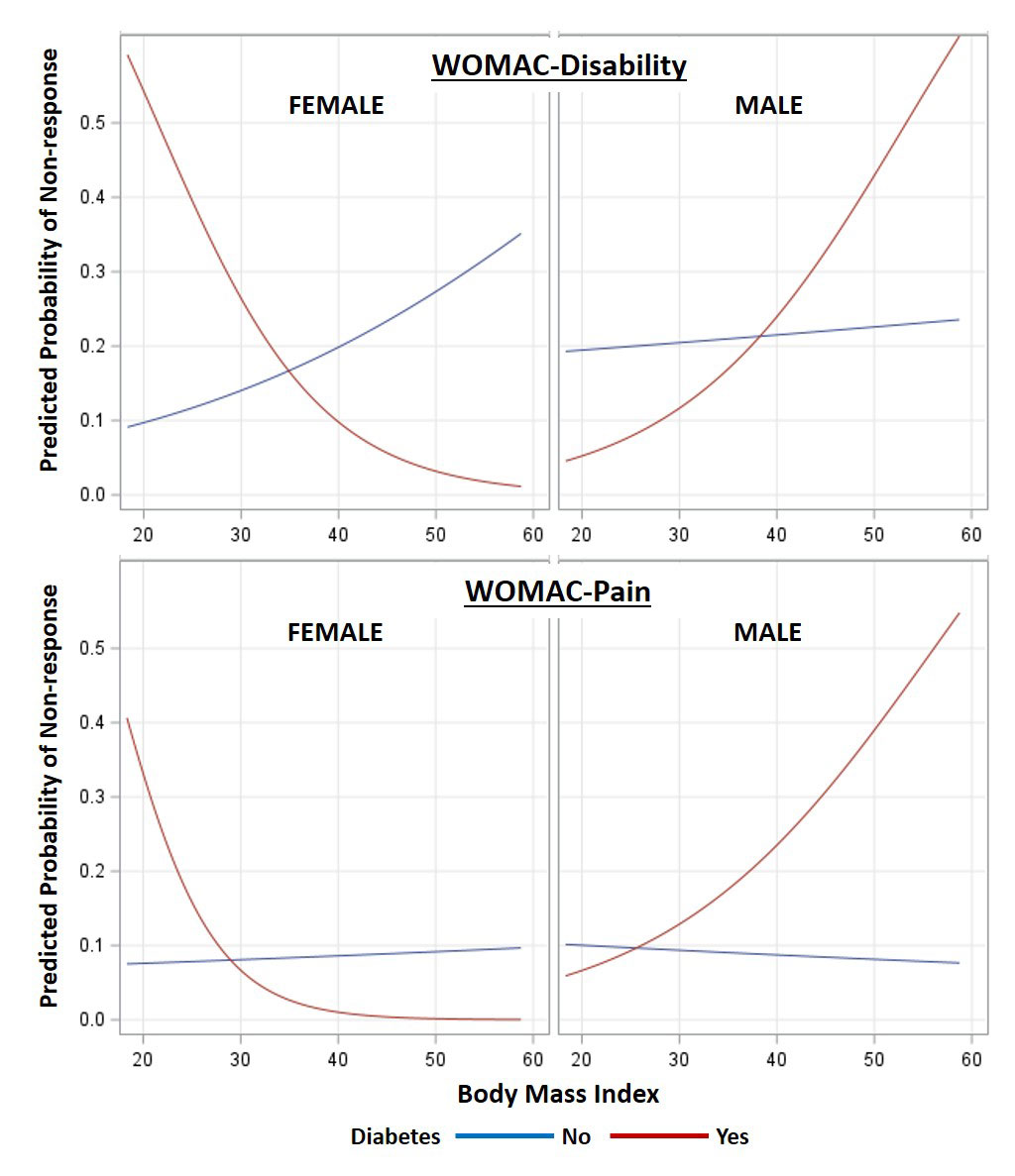
Results: The sample (626 hip, 754 knee) was 54.9% female, had a mean BMI of 30.1 (44.9% obese), and 13% reported diabetes. Among those with diabetes, non-response for disability and pain was 18.3% and 8.0% respectively, compared to 13.4% and 5.8% among those without. These crude non-response rates masked significant differences in diabetes impact by sex and BMI. From adjusted analyses for both disability and pain, a significant 3-way interaction (p=0.006 and 0.0394, respectively) between diabetes, sex, and BMI was found. Figure 1 displays the probabilities of non-response by sex, diabetes and BMI for knees. For example, the probability of non-response increased with increasing BMI in men with diabetes, but decreased with increasing BMI in women in diabetes. Findings were similar for hip patients.
Conclusion: Results suggest that variability in findings in the limited available literature may be due to differential impacts of diabetes on TJA outcomes depending on BMI and sex. The nature of these effects suggests that a simple consideration of the potential impact of diabetes as present vs. absent may not be sufficient, with implications for individual patients and the large clinical OA population undergoing joint arthroplasty.
To cite this abstract in AMA style:
Power J, Perruccio A, Davey J, Gandhi R, Mahomed N, Syed K, Veillette C, Rampersaud Y. The Impact of Diabetes Status on Pain and Disability Following Total Joint Arthroplasty for Hip and Knee Osteoarthritis: Variation by Sex and Body Mass Index [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/the-impact-of-diabetes-status-on-pain-and-disability-following-total-joint-arthroplasty-for-hip-and-knee-osteoarthritis-variation-by-sex-and-body-mass-index/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-impact-of-diabetes-status-on-pain-and-disability-following-total-joint-arthroplasty-for-hip-and-knee-osteoarthritis-variation-by-sex-and-body-mass-index/