Session Information
Date: Tuesday, November 14, 2023
Title: (2370–2386) Vasculitis – ANCA-Associated Poster III: Biomarkers & Renal Outcomes
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Older adults with ANCA-associated vasculitis (AAV) have distinct clinical presentations and outcomes when compared to younger adults. Despite a high incidence of AAV in older adults, they are underrepresented in clinical trials. Studies have focused on age as a risk factor for poor outcomes. Frailty, a syndrome associated with increased morbidity and mortality, has not been adequately studied in older adults with AAV and provides a more holistic assessment.
The objective of this study was to compare the impact of age and frailty on early (≤ 2 years of diagnosis) end-stage renal disease (ESRD), severe infection, and death in adults with incident AAV who are ≥ 75 years old vs 65-74 years old.
Methods: Patients ≥ 65 years were included from the 2002-2019 Mass General Brigham AAV cohort, a consecutive inception cohort. EGPA patients were excluded. Covariates including demographics, disease characteristics, and the Charlson comorbidity index were assessed at baseline. Disease activity at diagnosis was assessed using the Birmingham Vasculitis Activity Score (BVAS/GPA). Baseline frailty was measured using the claims-based frailty index (CFI); pre-established cut-offs defined degrees of frailty (robust, pre-frail, mildly frail, and moderately/severely frail).1
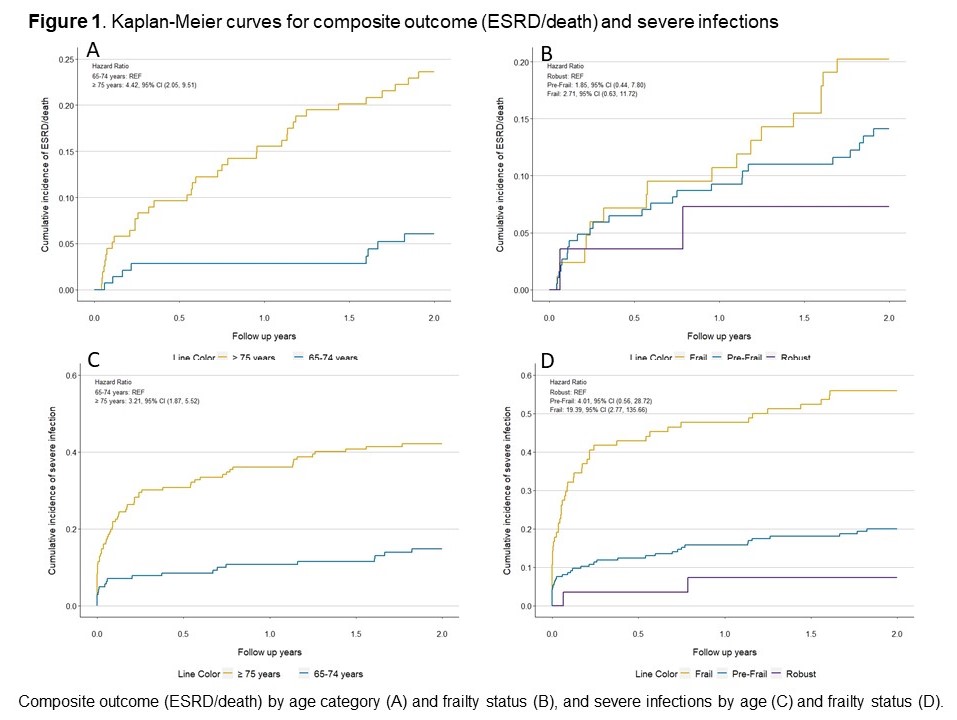
Death and ESRD (composite outcome) were ascertained from linkage to national registries and/or medical records. Severe infections were identified utilizing inpatient data or as a code in death certificate. The cumulative incidence of the death/ESRD and severe infections at 2-years were estimated. Kaplan-Meier curves for the probability of composite outcome and severe infection by age and frailty were generated. Multivariable analysis was performed to compare the association of age and frailty with death/ESRD and severe infections within 2 years of treatment initiation.
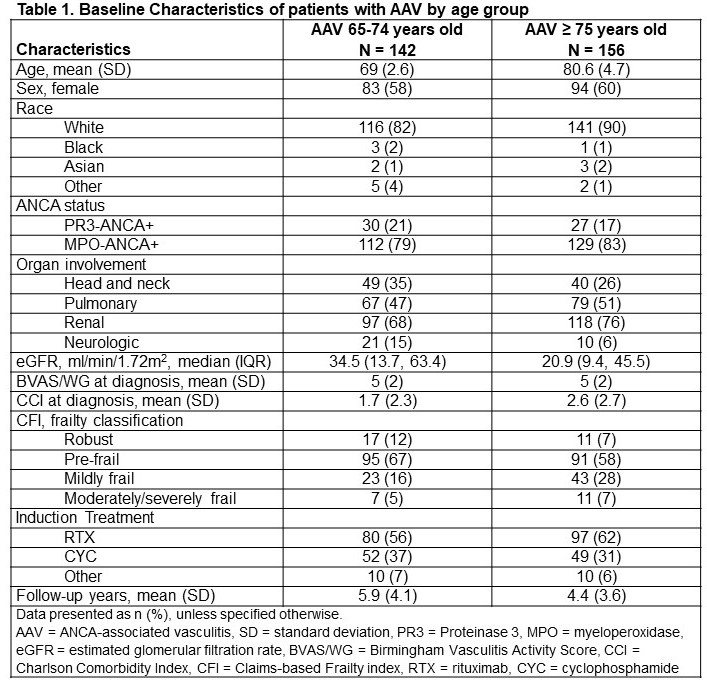
Results: There were 298 patients included. Most were female (61%), white (86%), MPO-ANCA+ (80%), and had renal involvement (72%). Patients ≥ 75 years old (n=156) had a median age of 81 years, while median age was 69 years in the 65-74 years group (Table 1).
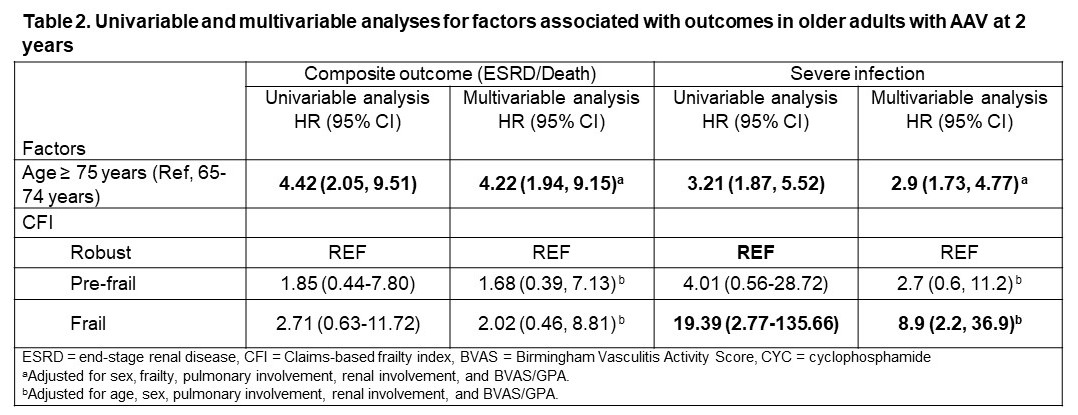
The cumulative incidence at 2 years of death/ESRD (23.1% [95% CI 16.5, 29.7]) vs 5.6% [95% CI 1.8, 9.4]) and severe infection (34.0% [95% CI 26.5, 41.4] vs 12% [95% CI 6.6, 17.3]) were higher in AAV patients ≥ 75 vs 65-74 years old. In the multivariable analysis, age ≥ 75 years was associated with an increased risk of composite outcome (hazard ratio (HR) 4.22, 95% CI 1.94-9.15); frailty was not (HR 2.02, 95% CI 0.46,8.81) (Table 2, Figure 1). In contrast, both frailty (HR 8.9, 95% CI 2.20,36.90) and age ≥ 75 years (HR 2.90, 95 CI% 1.73, 4.47) appeared to be independent risk factors for severe infections at 2-year follow-up; the association with frailty appeared greater.
Conclusion: AAV patients aged ≥ 75 vs 65-74 years had a higher incidence of death/ESRD and severe infections. Older age was associated with death/ESRD and severe infection risk. Frailty was a strong risk factor, independent of age, for severe infection. These findings highlight the need for innovative considerations beyond age when assessing outcome risks in older adults with AAV.
References
1. Kim DH, et al. J Gerontol A Biol Sci Med Sci
AAV = ANCA-associated vasculitis, SD = standard deviation, PR3 = Proteinase 3, MPO = myeloperoxidase, eGFR = estimated glomerular filtration rate, BVAS/WG = Birmingham Vasculitis Activity Score, CCI = Charlson Comorbidity Index, CFI = Claims-based Frailty index, RTX = rituximab, CYC = cyclophosphamide
ESRD = end-stage renal disease, CFI = Claims-based frailty index, BVAS = Birmingham Vasculitis Activity Score, CYC = cyclophosphamide
aAdjusted for sex, frailty, pulmonary involvement, renal involvement, and BVAS/GPA.
bAdjusted for age, sex, pulmonary involvement, renal involvement, and BVAS/GPA.
Composite outcome (ESRD/death) by age category (A) and frailty status (B), and severe infections by age (C) and frailty status (D).
To cite this abstract in AMA style:
Sattui S, Fu X, Cook C, Srivatsan S, Zhang Y, Wallace Z. The Impact of Chronologic versus Biologic Age on the Risk of Severe Infection, End-Stage Renal Disease, and Death in Older Adults with ANCA-Associated Vasculitis [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/the-impact-of-chronologic-versus-biologic-age-on-the-risk-of-severe-infection-end-stage-renal-disease-and-death-in-older-adults-with-anca-associated-vasculitis/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-impact-of-chronologic-versus-biologic-age-on-the-risk-of-severe-infection-end-stage-renal-disease-and-death-in-older-adults-with-anca-associated-vasculitis/