Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Our aim is to explore whether clinical features and long-term outcomes depend on autoantibodies in juvenile- and adult-onset systemic sclerosis (SSc), since they were not fully elucidated.
Methods: Autoantibodies, clinical characteristics, and cumulative survival rates for a maximum of 20 years were retrospectively analyzed in data from the Kyoto University Registry (juvenile-SSc [under 18 years old], n=17; adult-SSc, n=487) by Mann-Whitney U test, Fisher exact test, log-rank test, disease duration adjusted Cox proportional hazard analyses.
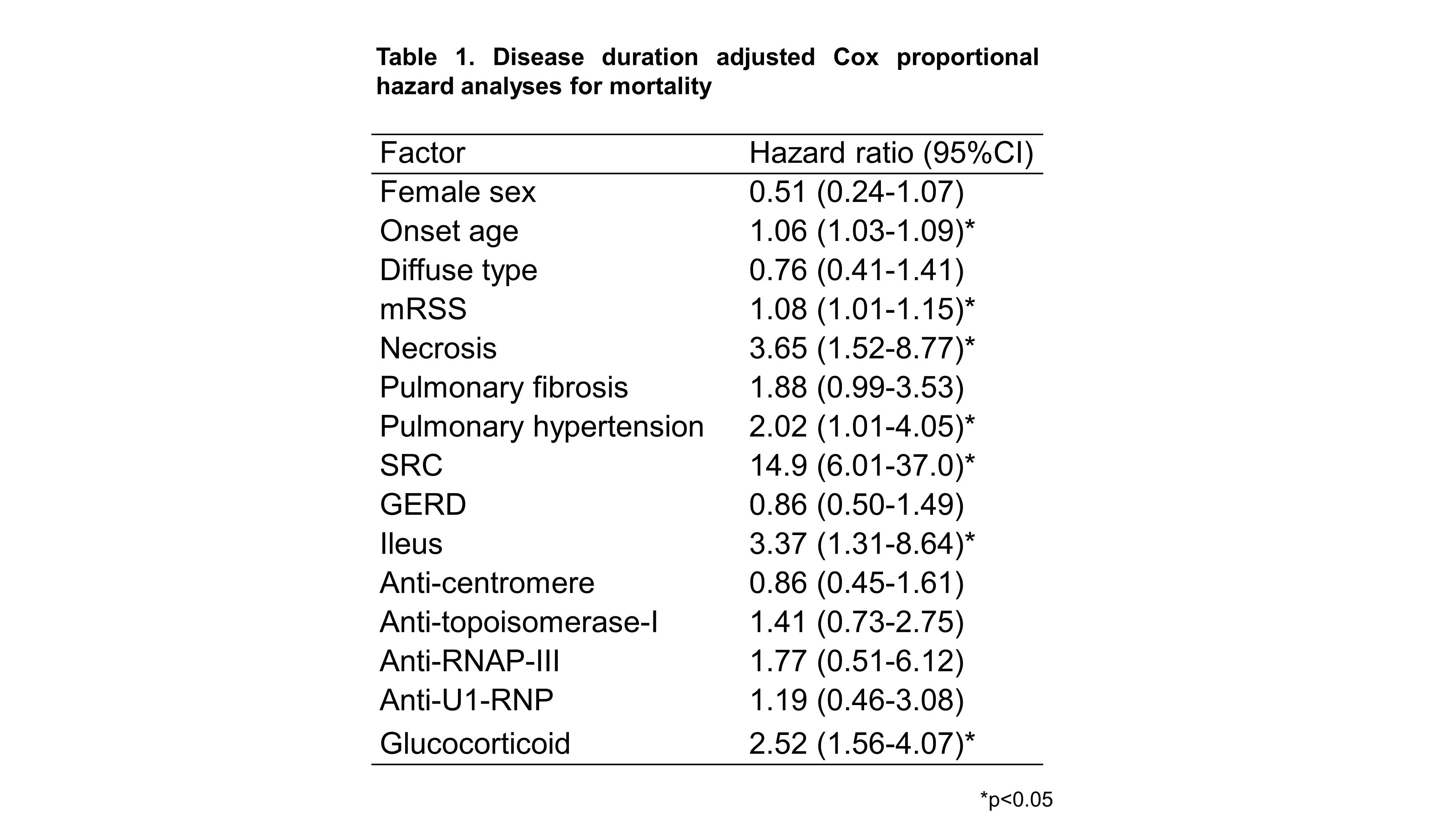
Results: The onset age was 14.9±3.8 years old for juvenile-SSc and 54.5±13.9 years old for adult-SSc. Higher levels of modified Rodnan Skin Score (mRSS) (juvenile-SSc vs. adult-SSc, 23.8±12.7 vs. 14.5±8.06, p=0.004) and higher frequencies of diffuse cutaneous SSc (88% vs. 48%, p=0.0001) and ileus (18% vs. 3%, p=0.02) were observed in juvenile-SSc compared to adult-SSc (Figure 1). In juvenile-SSc, anti-topoisomerase-I was the most frequent and followed by anti-centromere: autoantibodies were detected as anti-topoisomerase-I (juvenile-SSc vs. adult-SSc, 75% vs. 26%), anti-centromere (24% vs. 54%), and anti-RNA polymerase-III (RNAP-III, 0% vs. 12%). Diffuse cutaneous SSc and multi-organ involvement were observed in anti-topoisomerase-I compared to anti-centromere in both juvenile-SSc and adult-SSc. Furthermore, anti-RNAP-III in adult-SSc was associated with a higher incidence of scleroderma renal crisis (SRC, 18%) compared to anti-topoisomerase-I and anti-centromere.
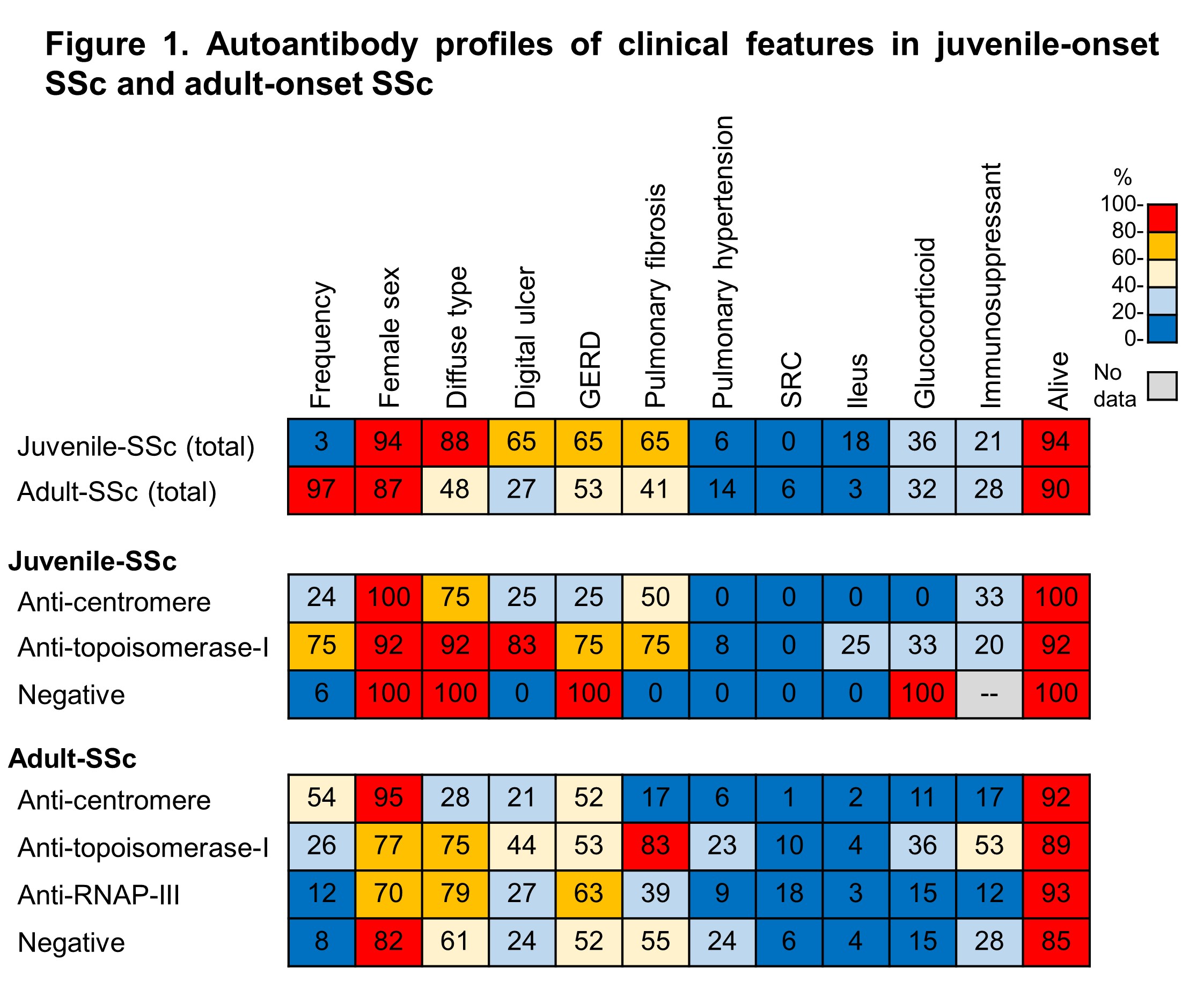
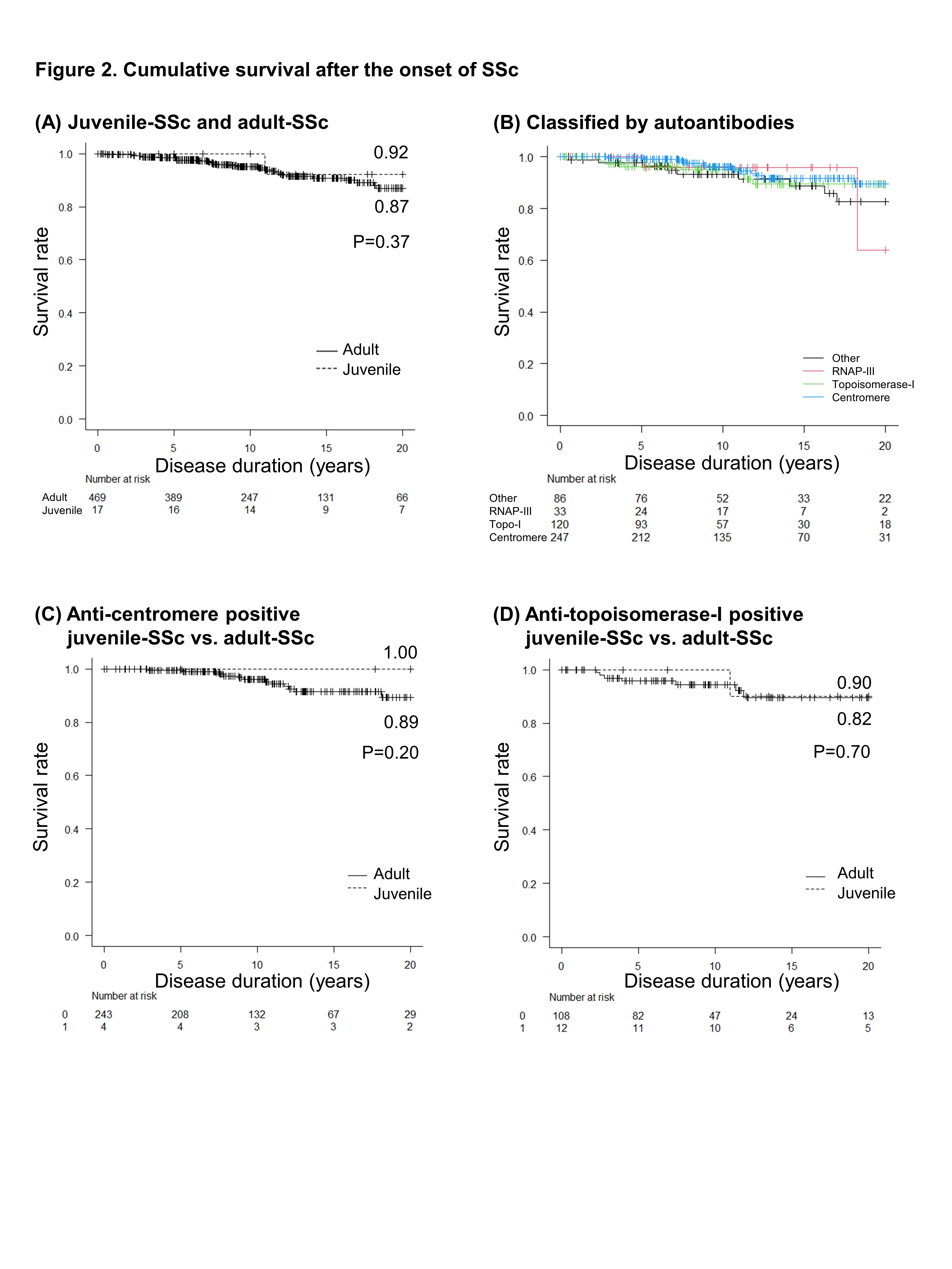
Treatments were not different between juvenile-SSc and adult-SSc: glucocorticoid (juvenile-SSc vs. adult-SSc, 29% vs. 21%, p=0.39), and immunosuppressants (21% vs. 28%, p=0.76). A total of 41 patients died during 20 years, including 1 juvenile patient with anti-topoisomerase-I. Causes of death were scleroderma-related (51%), malignancy (27%), infection (10%), and others (12%). Cumulative survival rates by Kaplan-Meier curve were not different between juvenile-SSc (92%) and adult-SSc (87%) (p=0.36 by log-rank test) (Figure 2A). Cumulative survival classified by autoantibodies were not different significantly: anti-centromere (89.6%), anti-topoisomerase-I (89.4%), other (82.6%), and anti-RNAP-III (63.9%) (Figure 2B). There were no significant differences between juvenile-SSc and adult-SSc when they were classified by anti-centromere or anti-topoisomerase-I (Figure 2C, 2D). By cox proportional hazard analyses for death, onset age (hazard ratios: 1.062, 95% confidence interval: 1.034-1.091), pulmonary hypertension (2.02, 1.01-4.05), SRC (14.9, 6.01-37.0), ileus (3.37, 1.31-8.64), necrosis (3.65, 1.52-8.77), and glucocorticoid use (2.52, 1.56-4.07) were associated with death (Table 1). In contrast, hazard ratios of autoantibodies for death were not significant.
Conclusion: Compared to adult-SSc, juvenile-SSc had higher frequencies of diffuse cutaneous SSc and anti-topoisomerase-I, and lower frequency of anti-centromere. Older age was associated with mortality, while there were no differences between autoantibodies.
Autoantibody profiles of clinical features in juvenile-onset SSc and adult-onset SSc
(A) Juvenile-SSc and adult-SSc; (B) Classified by autoantibodies; (C) anti-centromere positive juvenile-SSc vs. adult-SSc; (D) anti-topoisomerase-I positive juvenile-SSc vs. adult-SSc, log-lank test.
To cite this abstract in AMA style:
Tsuji H, Hiwa R, Shirakashi M, Akizuki S, Nakashima R, Onishi A, Yoshifuji H, Tanaka M, Morinobu A. The Association of Autoantibodies with Clinical Manifestations and Long-term Outcomes in Juvenile- and Adult-onset Systemic Sclerosis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/the-association-of-autoantibodies-with-clinical-manifestations-and-long-term-outcomes-in-juvenile-and-adult-onset-systemic-sclerosis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-association-of-autoantibodies-with-clinical-manifestations-and-long-term-outcomes-in-juvenile-and-adult-onset-systemic-sclerosis/