Session Information
Session Type: Abstract Session
Session Time: 1:00PM-1:15PM
Background/Purpose: Multimorbidity, the presence of multiple chronic conditions, is over-represented in RA. A cardiometabolic multimorbidity (CMM) phenotype has emerged in the general population, but is not well studied in RA despite cardiovascular disease (CVD) being the leading cause of death in RA. We evaluated the risk of CMM in RA and whether CMM risk has improved with advances in RA management.
Methods: Using national Veterans Affairs (VA) data, we identified incident RA patients (≥2 RA ICD codes, rheumatologist diagnosis, positive autoantibody or DMARD fill, plus ≥365 days in VA care before a DMARD fill or RA ICD code) matched up to 10 non-RA controls on age, sex, and VA enrollment year. Cohort entry was the date the RA algorithm was fulfilled. A traditional CMM outcome included coronary artery disease (CAD), stroke, and diabetes (DM). Given the growing recognition of Cardiovascular-Kidney-Metabolic (CKM) syndrome and its impact on both atherosclerotic CVD and heart failure (HF), an expanded CMM outcome was defined, informed by CKM syndrome components (CAD, stroke, HF, DM, hypertension [HTN], hyperlipidemia [HPL], chronic kidney disease [CKD], and obesity). Individual conditions were identified by ≥2 ICD codes ≥30 days apart. CMM onset was the date ≥2 conditions developed. We additionally defined more severe CMM phenotypes, requiring ≥3 and ≥5 (expanded CMM only) conditions. Patients meeting CMM outcomes prior to cohort entry were excluded. We examined the RA-related risk of CMM using Cox regression, stratified on matched sets and adjusting for age, sex, race, ethnicity, smoking status, BMI, rurality, and healthcare utilization. Censoring occurred at death or end of study period (1/2023). Temporal trends in CMM risk were evaluated in models stratified on RA diagnosis year (2000-2005, 2006-2011, 2012-2017), testing the linear interaction of RA status and time-period. Secondary analyses evaluated CMM risk stratified by seropositivity (RF and/or anti-CCP) and elevated inflammation (ESR and/or CRP) at baseline.
Results: We matched 28,537 RA patients (mean age 63, 85% male) to 252,602 non-RA controls. Over 2,522,982 person-years, 25,474 patients developed the traditional CMM outcome. The incidence of all CMM outcomes was higher in patients with RA (range aHR 1.14-1.31) in fully adjusted models (Table 1). The RA-related risk of CMM was higher in more recent time periods (p-for-trend < 0.001 for all CMM outcomes; Figure 1). The expanded CMM outcome severe phenotype (≥5 conditions) in the most recent time-period (RA diagnosis year 2012-17) was the most over-represented outcome in RA (aHR 1.42 [1.34-1.51]; Figure 1). CMM risk compared to controls was similar regardless of serostatus, while risk was typically accentuated in those with elevated inflammation (range aHR 1.13-1.48) at baseline compared to those with normal inflammatory measures (range aHR 1.12-1.18) (Table 2).
Conclusion: RA-related risk of CMM is worsening over the past two decades despite advances in RA disease activity management. The burden of CMM highlighted by these data underscores the need for additional RA-specific strategies paired with disease activity control to reduce cardiometabolic risk and improve CVD-related outcomes in this high-risk population.
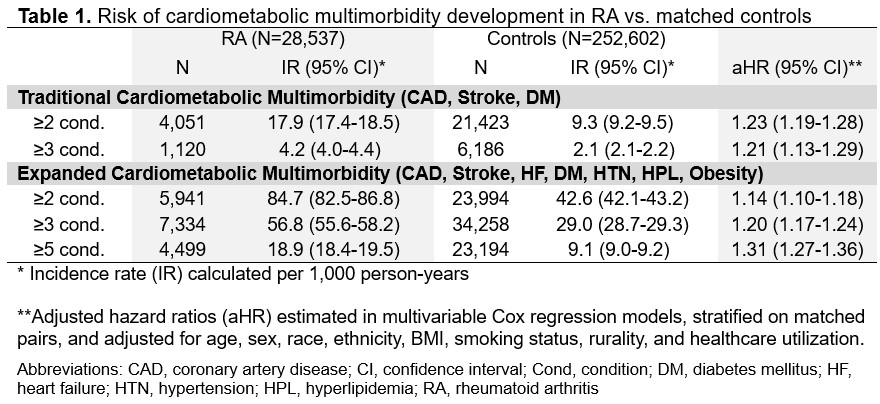 Table 1. Risk of cardiometabolic multimorbidity development in RA vs. matched controls
Table 1. Risk of cardiometabolic multimorbidity development in RA vs. matched controls
.jpg) Figure 1. Temporal trends in the risk of cardiometabolic multimorbidity in RA vs. matched controls.
Figure 1. Temporal trends in the risk of cardiometabolic multimorbidity in RA vs. matched controls.
.jpg) Table 2. Risk of cardiometabolic multimorbidity in RA, stratified by seropositivity and baseline acute phase reactants
Table 2. Risk of cardiometabolic multimorbidity in RA, stratified by seropositivity and baseline acute phase reactants
To cite this abstract in AMA style:
Johnson T, Baker J, Roul P, Cannon G, Kunkel G, Sauer B, Mikuls T, England B. Temporal Trends in Cardiometabolic Multimorbidity Risk in Rheumatoid Arthritis: A National, Matched Cohort Study [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/temporal-trends-in-cardiometabolic-multimorbidity-risk-in-rheumatoid-arthritis-a-national-matched-cohort-study/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/temporal-trends-in-cardiometabolic-multimorbidity-risk-in-rheumatoid-arthritis-a-national-matched-cohort-study/
