Session Information
Date: Sunday, November 12, 2023
Title: Abstracts: Systemic Sclerosis & Related Disorders I: Translational
Session Type: Abstract Session
Session Time: 2:00PM-3:30PM
Background/Purpose: Peripheral blood leukocyte telomere length (PBL-TL) has been associated with disease and organ specific morbidity and mortality in conditions associated with pulmonary fibrosis including connective tissue disorders. TL shortening has been implicated in SSc-related interstitial lung disease (ILD), but its association with other organ involvement, disease severity, and overall survival remains unknown. The goal of this study was to define the relationship of PBL-TL with SSc-specific disease manifestations and clinical outcomes including mortality.
Methods: A retrospective longitudinal cohort study was performed using a large, well characterized cohort of SSc patients fulfilling the ACR/EULAR 2013 classification criteria and healthy controls (HC). PBL-TL was measured by quantitative PCR from DNA isolated from the blood. Age adjusted TL was calculated using linear regression of TL from HC. Multivariate modeling was utilized to assess the association of PBL-TL with SSc disease presence and severity of skin thickening, ILD, pulmonary arterial hypertension (PAH), peripheral vascular disease (PVD), and event free survival (lung transplantation and/or death) from disease onset and time of TL measurement. To assess concordance of findings between blood and SSc target tissues, TL was measured in skin and lung tissue by telomere fluorescence in situ hybridization (Telo-FISH) in SSc and HC, and compared using Wilcoxon rank-sum test.
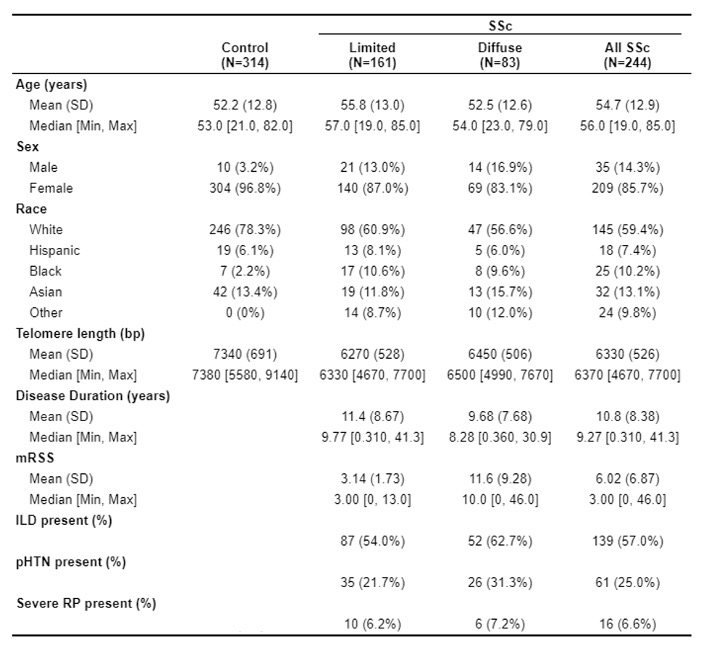
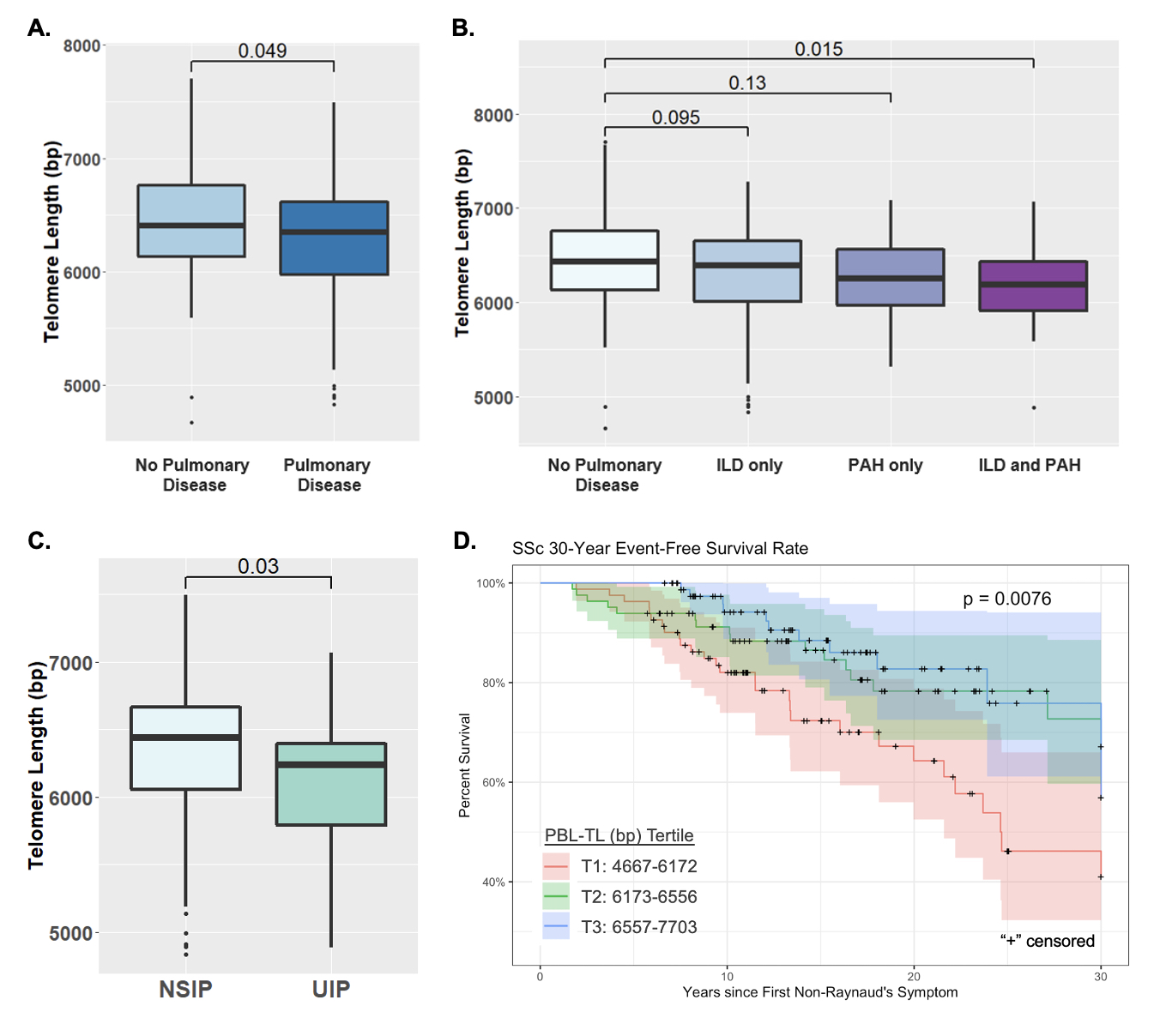
Results: 558 participants (244 SSc and 314 controls) were included in this study (Table 1). PBL-TL was significantly shorter in SSc than healthy controls. In multivariate modeling, controlling for age, sex, race, smoking, disease duration and autoantibody status, shortened TL was significantly associated with presence of SSc related pulmonary involvement (OR 1.98 per 1000bp shortening, p=0.03) (Fig1A). PBL-TL was not associated with SSc skin disease (p=0.21) or PVD (p=0.20). Within pulmonary disease, TL shortening was strongly associated with ILD presence (OR 2.21, p =0.009). The shortest PBL-TL was found in subjects with concurrent ILD and PAH (Fig 1B). Shortened TL was also associated with lung disease severity including lower DLCO% (p=0.006) and UIP pattern by chest CT compared to NSIP (p=0.03, Fig 1c). Patients requiring hospitalization for respiratory or right ventricular failure had shorter TL (6169±434 vs. 6350±535, p=0.02) and TL shortening was associated with worse event free survival among all SSc patients from both time of TL measurement (p=0.03) and disease onset (p=0.008) (Figure 1D). TL was shorter in type II alveolar cells in lung tissues from SSc-ILD patients compared to healthy controls (p=0.014). In contrast, no difference was found in TL in epidermal cells (KRT5+) of skin (p=0.82).
Conclusion: This cohort study found a strong association between TL measured in the peripheral blood of SSc patients and more severe pulmonary involvement, particularly with concurrent ILD/PAH, and worse clinical outcomes including increased hospitalization due to respiratory failure as well as worse survival. This study provides rationale to further investigate the role of telomere dysfunction in SSc-ILD pathogenesis and to validate TL as a potentially useful biomarker in SSc.
To cite this abstract in AMA style:
Yang M, Liu S, Lee S, French S, Wolters P, Boin F. Telomere Length of Peripheral Blood Cells Predicts More Severe Pulmonary Disease and Worse Survival in Systemic Sclerosis [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/telomere-length-of-peripheral-blood-cells-predicts-more-severe-pulmonary-disease-and-worse-survival-in-systemic-sclerosis/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/telomere-length-of-peripheral-blood-cells-predicts-more-severe-pulmonary-disease-and-worse-survival-in-systemic-sclerosis/