Session Information
Date: Monday, November 13, 2023
Title: (1100–1123) Metabolic & Crystal Arthropathies – Basic & Clinical Science Poster II
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Despite rheumatology guidelines’ emphasis on treat-to-target-serum-urate (SU) levels (<6 or <5 mg/dL, urate crystal sub-saturation points), this pathophysiology-based recommendation is not accepted in primary care practice (where >90% of gout care occurs) or endorsed by the American College of Physicians.To that end, proportions of gout flares associated with these target levels, including those requiring hospitalization, are unknown. We quantified associations of target SU with recurrent flares, including gout-primary hospitalizations, among gout patients nested in a prospective nationwide cohort.
Methods: This was a prospective cohort study of UK adults recruited over 2006-2010 and followed-up through primary care medical record linkage. As done previously [Cipolletta et al. JAMA 2022], flares among prevalent gout patients were ascertained by (1) hospitalization with gout (ICD-10 M10) as primary discharge diagnosis; (2) diagnosis of gout flare in primary care records; or (3) diagnosis of gout in primary care records and prescription issued on the same day for corticosteroids, colchicine, or non-steroidal anti-inflammatory drugs (NSAIDs).We also investigated flares requiring hospitalisation. Poisson regression was used to assess the relation between baseline SU levels and rates of recurrent gout flares over 1, 2, 5, and 10 years of follow-up.
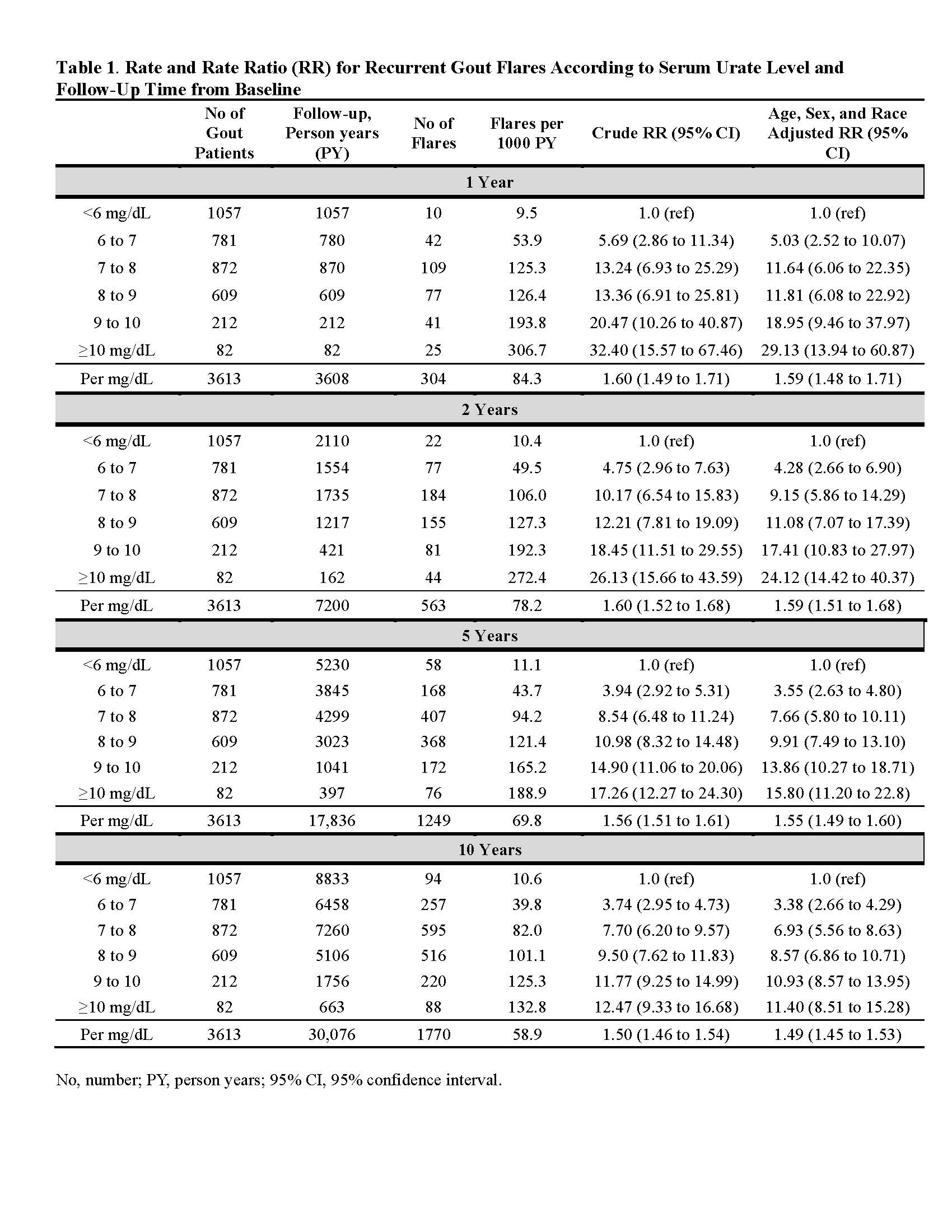
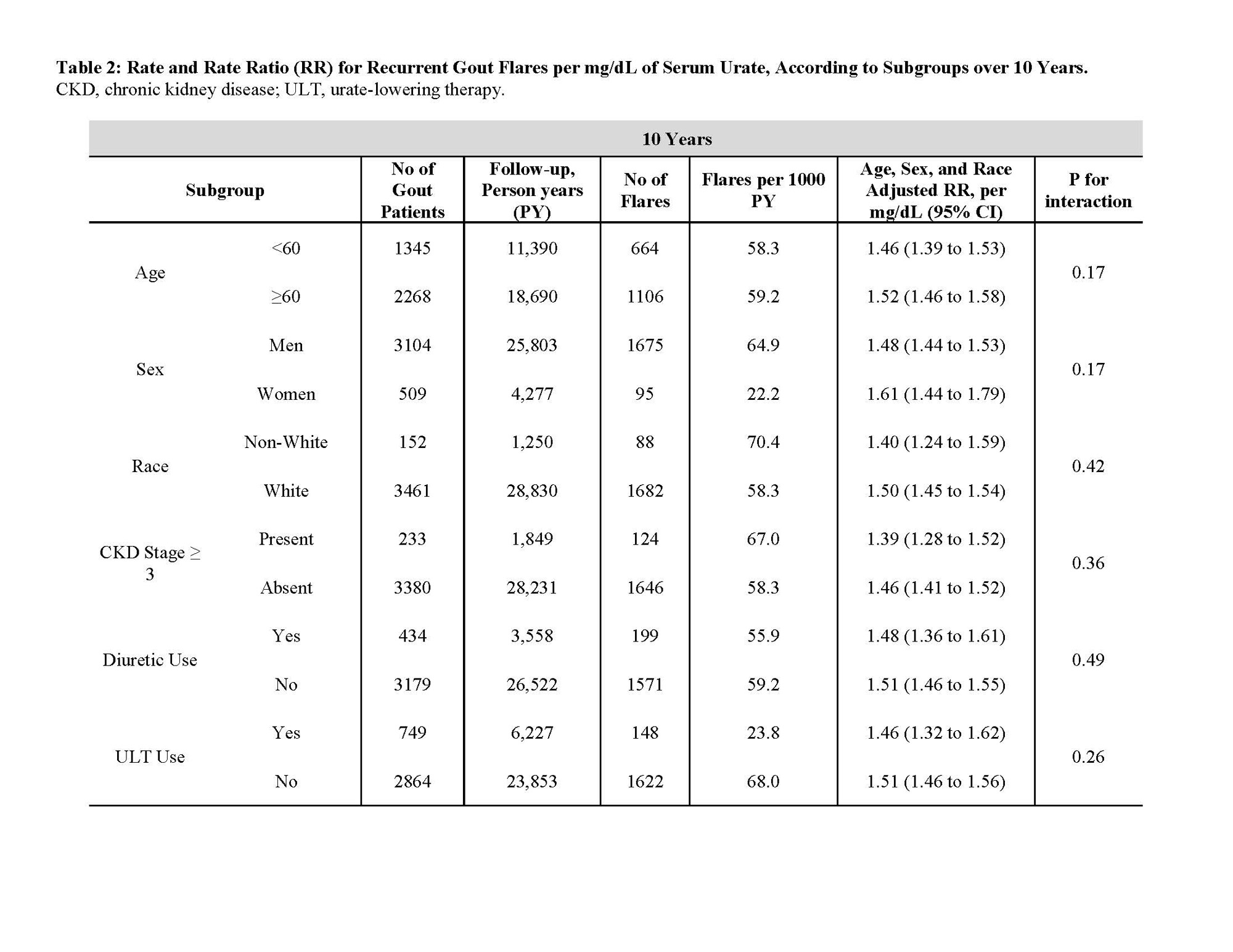
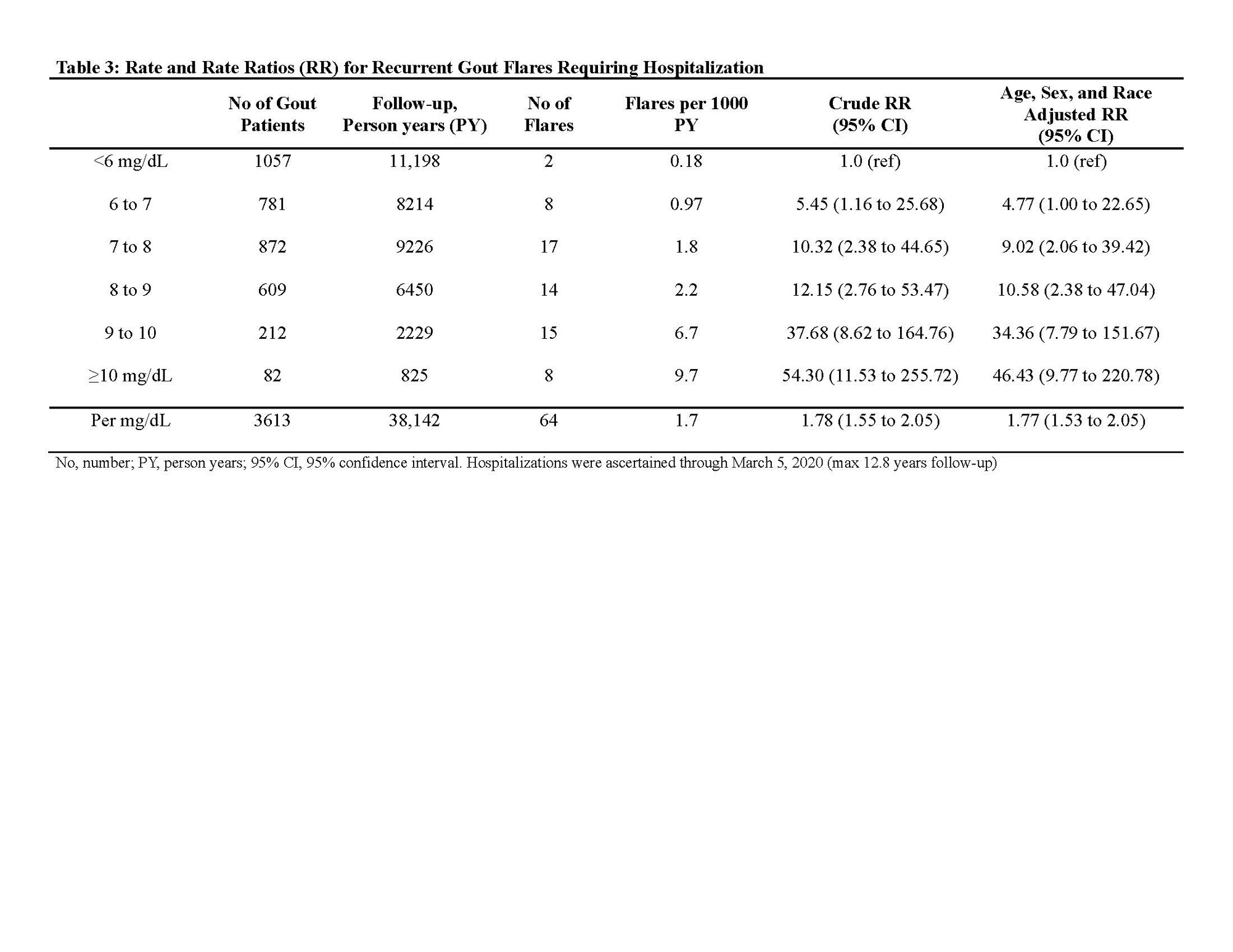
Results: We followed 3,613 prevalent gout patients (86% male, mean age 60 years), among whom we documented 1,770 gout flare events over 10 years.95% (1,676/1,770) and 98% (1,728/1,770) of flares occurred in baseline SU ≥6 and ≥5 mg/dL, respectively. Rate ratio (RR) for flares with SU levels of < 6.0, 6.0-6.9, 7.0-7.9, 8.0-8.9, 9.0-9.9, and ≥10 mg/dL were 1.0, 5.03, 11.64, 11.81, 18.95, and 29.13, respectively during first year of follow-up (1.59 [1.48-1.71] per mg/dL), and 1.0, 3.38, 6.93, 8.57, 10.93, and 11.40, respectively, over whole 10-year follow-up (1.49 [1.45-1.53] per mg/dL) (Table 1).Associations persisted irrespective of sex, race, age group, chronic kidney disease status, and diuretic and urate-lowering therapy use (all P for interaction >0.17) (Table 2). 97% (62/64) and 100% (64/64) of flares requiring hospitalization occurred in baseline SU ≥6 and ≥5 mg/dL, respectively (Table 3); corresponding RR were 1.0, 4.77, 9.02, 10.58, 34.36, and 46.43, respectively (1.77 [1.53-2.05] per mg/dL).
Conclusion: In this prospective cohort of gout patients treated in primary care, 95% and 98% of flares occurred in baseline SU ≥6 and ≥5 mg/dL, respectively. Associations were more prominent for hospitalized flares, with no cases among those with SU < 5mg/dL; higher serum urate levels are strongly associated with frequency of recurrent flares in a graded manner. These findings support the utility of these target urate levels for gout patient care, consistent with a treat-to-target approach recommended by rheumatology societies in the US and Europe, but not the American College of Physicians.
No, number; PY, person years; 95% CI, 95% confidence interval.
CKD, chronic kidney disease; ULT, urate-lowering therapy; SD, standard deviation.
No, number; PY, person years; SD, standard deviation; 95% CI, 95% confidence interval. Hospitalizations were ascertained through March 5, 2020 (max 12.8 years follow-up)
To cite this abstract in AMA style:
McCormick N, Yokose C, Challener G, Joshi A, Tanikella S, Choi H. Target Serum Urate Levels, Recurrent Gout Flare Rates, and Gout-Primary Hospitalizations: Nationwide Prospective Cohort Study of 3,613 Gout Patients [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/target-serum-urate-levels-recurrent-gout-flare-rates-and-gout-primary-hospitalizations-nationwide-prospective-cohort-study-of-3613-gout-patients/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/target-serum-urate-levels-recurrent-gout-flare-rates-and-gout-primary-hospitalizations-nationwide-prospective-cohort-study-of-3613-gout-patients/