Session Information
Session Type: ACR Concurrent Abstract Session
Session Time: 4:30PM-6:00PM
Synovial Tissue Resident Macrophages Play the protective role in the Development of Inflammatory Arthritis in CD11c-Flip-KO Mice
Qi-Quan Huang1, Renee Doyle1, Robert Birkett1 and Richard M. Pope1
Background/Purpose: We have generated a CD11c-Flip-KO (HUPO) mouse line that spontaneously develops erosive arthritis resembling rheumatoid arthritis. Arthritis spontaneously developed beginning at 5weeks of age in ~10% of HUPO, progressing to ~80% incidence at ≥20 weeks. HUPO mice crossed with Rag-/- mice developed a mild non-progressive arthritis due to macrophage infiltration, supporting an important role for macrophages in disease pathogenesis. This study examined the phenotype of macrophages in the joints of littermate control mice and of ≥ 20 week old HUPO mice with and without arthritis.
Methods: Ankle joint cells were dissected and digested with collagenase. Cells were analyzed by flow cytometry employing multicolor fluorochrome-antibodies. Arthritis were evaluated by clinical score for the inflammation, joint deformity and grip strength, ranging from 0-28.
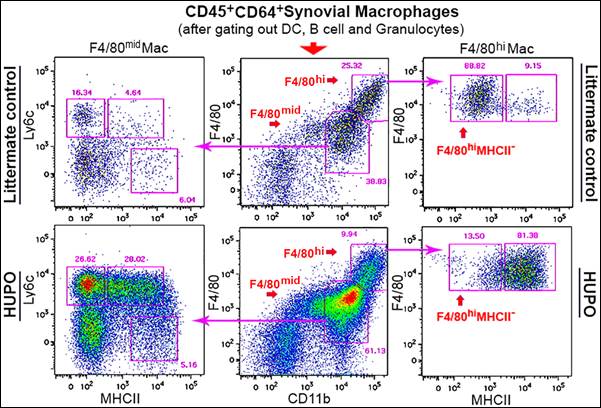
Results: Under homeostatic conditions in control mice synovial macrophages are defined as CD11b+CD64+F4/80+, about 90% co-express CD11c+. Further, macrophages may be defined as F4/80hi or F4/80mid (Figure). The F4/80mid Ly6C+ MHCII– are macrophages recently differentiated from peripheral blood monocytes. Increase of MHCII and loss of Ly6C represents progressive stages of macrophage differentiation. The percent F4/80mid Ly6C+ MHCII– macrophages were increased (p <0.001) in ankles of HUPO mice with arthritis, compared with littermate controls. The F4/80 hi macrophages are Ly6C–, and either MHCII+ or MHCII–. During homeostasis, the F4/80hi MHCII– macrophages are considered as tissue resident macrophages. F4/80hi MHCII– tissue resident macrophages are greatly reduced and F4/80hi MHCII+ macrophages increased (p < 0.01-0.001) in HUPO mice with arthritis, compared with littermate controls or HUPO mice without arthritis. F4/80hi MHCII– macrophages were also decreased in the joints of HUPO mice at 4 weeks, before arthritis onset. In HUPO mice the F4/80hi MHCII– macrophages were inversely correlated (p = 0.023) with arthritis severity, while the F4/80hi MHCII+ macrophages were positively correlated (p = 0.024). Further supporting the role of F4/80hi MHCII– macrophages in suppressing inflammation, the percent F4/80hi MHCII– macrophages was strongly, inversely correlated (r = -0.874, p<0.001) with the percent granulocytes in the synovial tissue.
Conclusion: In HUPO mice the reduction of synovial tissue resident macrophages, which are also CD11c+, was highly associated with inflammation and the onset and severity of arthritis. The influx of peripheral blood monocytes and their differentiation into macrophages was observed in HUPO arthritis. Approaches to preserve tissue resident macrophages or to decrease influx of peripheral blood monocytes may be effective therapeutically in HUPO, and potentially other forms of inflammatory arthritis.
To cite this abstract in AMA style:
Huang QQ, Doyle RE, Birkett R, Pope RM. Synovial Tissue Resident Macrophages Play the Protective Role in the Development of Inflammatory Arthritis in CD11c-Flip-KO Mice [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/synovial-tissue-resident-macrophages-play-the-protective-role-in-the-development-of-inflammatory-arthritis-in-cd11c-flip-ko-mice/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/synovial-tissue-resident-macrophages-play-the-protective-role-in-the-development-of-inflammatory-arthritis-in-cd11c-flip-ko-mice/