Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Patients with polyarticular JIA (pJIA) have a refractory disease course with increased risk for joint damage resulting in poor functional outcome and decreased quality of life. The highest risk is in patients who are younger at diagnosis. Therefore, it is important for patients to receive timely access to pediatric rheumatology for management. The objective of this study is to examine the association of social determinants of health (SDoH) on time from reported symptom onset (pain, joint stiffness, swelling) to first appointment with pediatric rheumatology in pJIA patients.
Methods: We retrospectively analyzed Childhood Arthritis and Rheumatology Research Alliance (CARRA) registry from July 2015 through February 2020. Inclusion criteria were USA residency and pJIA diagnosis with recorded >4 joints involved in first 6 months of disease, exclusion criteria were invalid zip code and additional diagnosis of systemic inflammatory or autoimmune disease. The SDoH we studied were family income, guardian’s highest level of education, and community poverty level. Demographics, approximate date of symptom onset, were queried. Five-digit zip-codes were used to extrapolate community poverty levels using 2014-2018 American Community Survey data. The Kaplan-Meier method was used to estimate rheumatology visit-free survival. The log-rank test was used to compare rheumatology visit-free survival between the SDoH. Cox proportional-hazards models were utilized to estimate hazard ratios for the outcome mentioned above, adjusted for age of diagnosis.
Results: 1684 patients fit criteria for this study. Demographics are listed in Table 1. Twenty percent of patients had missing time to first appointment. The median time from symptom onset to first pediatric rheumatology visit was 3 months (IQR: 1,6). Kaplan-Meier curves showing the probability of first rheumatology visit for time from symptom onset are shown in figure 1. Children with family reported income in the range of $25,000-49,999 were likely to have longer time to first appointment (unadjusted HR 0.76, CI 0.6-0.97, p = 0.025). These relationships remain consistent when additionally adjusted for age at diagnosis (table 2). Guardian’s highest level of education, and community poverty level did not affect the time to first appointment.
Conclusion: Family reported income, guardian education, and community poverty did not impact time to first appointment. Children within the income bracket of $25,000-49,999 may have less access to subspecialists, transportation, or advocacy compared to other children. Ascertainment bias into the registry may skew the cohort to a wealthy and educated population. Recall bias on symptom onset is possible. Future directions for research include stratification of community poverty levels and evaluation of public vs private insurance on time to first appointment.
 Table1: Patient Characteristics and demographics
Table1: Patient Characteristics and demographics
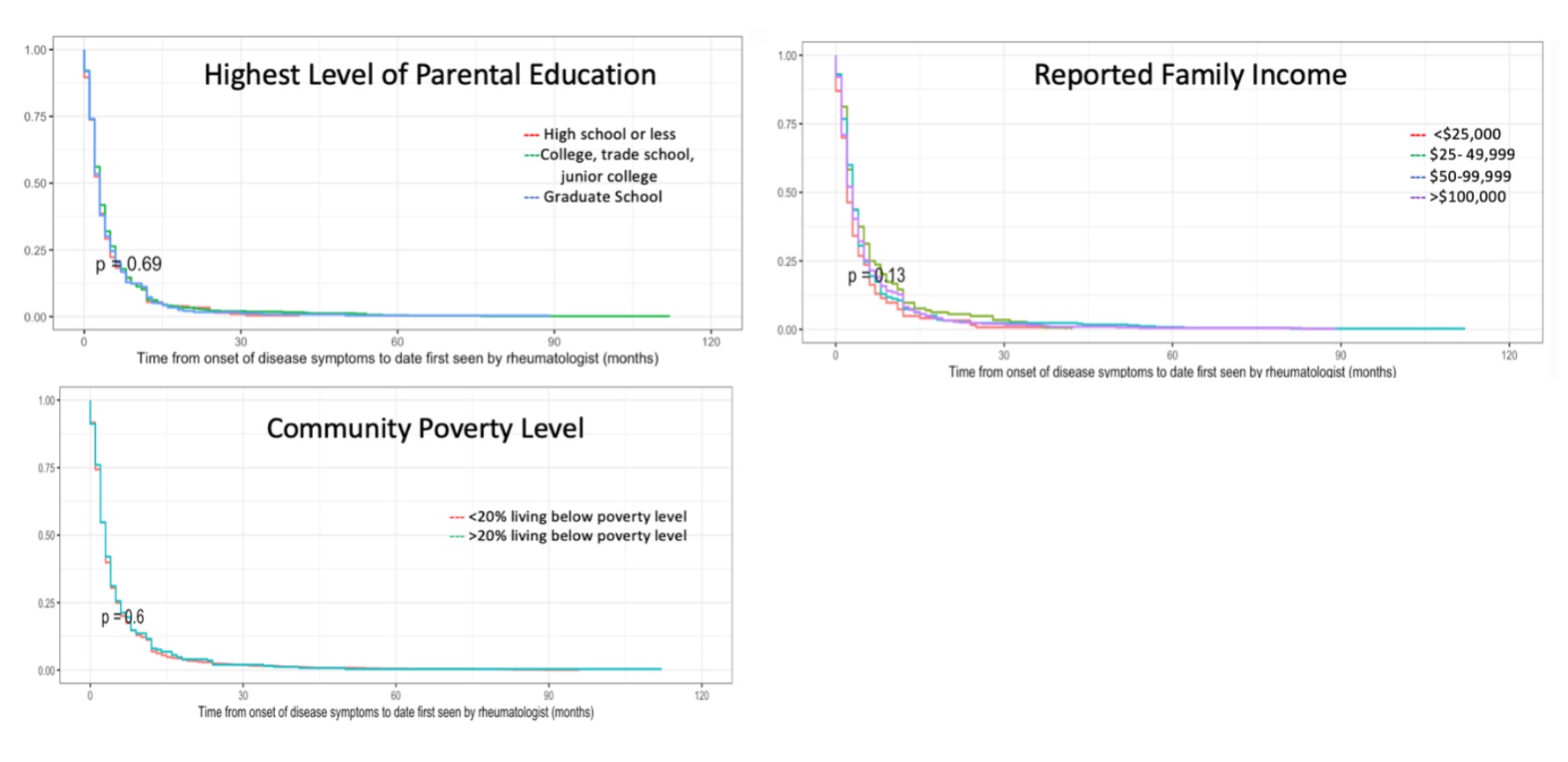 Figure 1: Kaplan- Meier curves for time from symptom onset to date first presentation to pediatric rheumatologist
Figure 1: Kaplan- Meier curves for time from symptom onset to date first presentation to pediatric rheumatologist
 Table 2: Association of social determinants of health with time to first presentation to pediatric rheumatologist
Table 2: Association of social determinants of health with time to first presentation to pediatric rheumatologist
To cite this abstract in AMA style:
Balmuri N, Cooley V, Gerber L, Goodman S, Mehta B, Onel K. Social Determinants of Health and Time to First Pediatric Rheumatology Appointment in Polyarticular Juvenile Idiopathic Arthritis [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/social-determinants-of-health-and-time-to-first-pediatric-rheumatology-appointment-in-polyarticular-juvenile-idiopathic-arthritis/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/social-determinants-of-health-and-time-to-first-pediatric-rheumatology-appointment-in-polyarticular-juvenile-idiopathic-arthritis/
