Session Information
Session Type: Poster Session B
Session Time: 9:00AM-10:30AM
Background/Purpose: There is a pressing need to identify novel therapeutic approaches and noninvasive biomarkers in lupus nephritis (LN). In this study, we quantified serum soluble mediators in the large Accelerating Medicines Partnership (AMP) LN longitudinal cohort to identify novel biomarkers of histological features and treatment response and provide insights into the pathogenesis of LN.
Methods: SLE patients meeting ACR or SLICC criteria (n=268) undergoing a clinically indicated kidney biopsy with a urine protein/creatinine (UPCR) ≥0.5 were recruited for this study as part of the AMP. Serum samples were collected from patients at the time of diagnostic kidney biopsy and 3-, 6-, and 12-months post-biopsy and from 22 healthy donors (HD). Concentrations of 51 analytes, including cytokines, chemokines, and TNFR superfamily members, were analyzed by xMAP multiplex assays on the Bio-Rad BioPlex200® array system. TACE levels were determined by ELISA. Clinical response was determined at 12-months post-biopsy using the Abatacept and Cyclophosphamide Combination Efficacy and Safety Study definitions in patients with a baseline UPCR >1.0 and International Society of Nephrology/Renal Pathology Society class III, IV, V, or combination thereof.
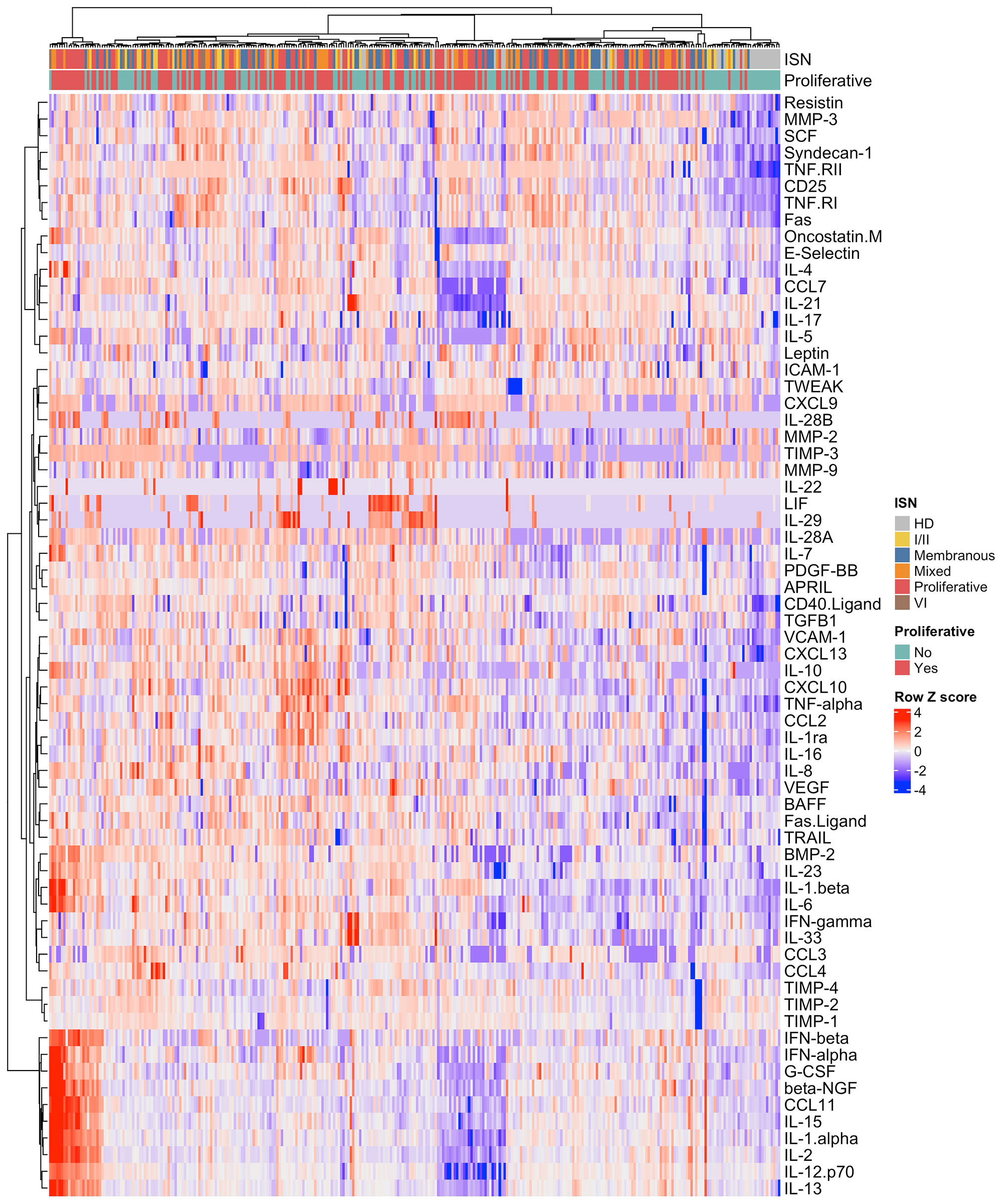
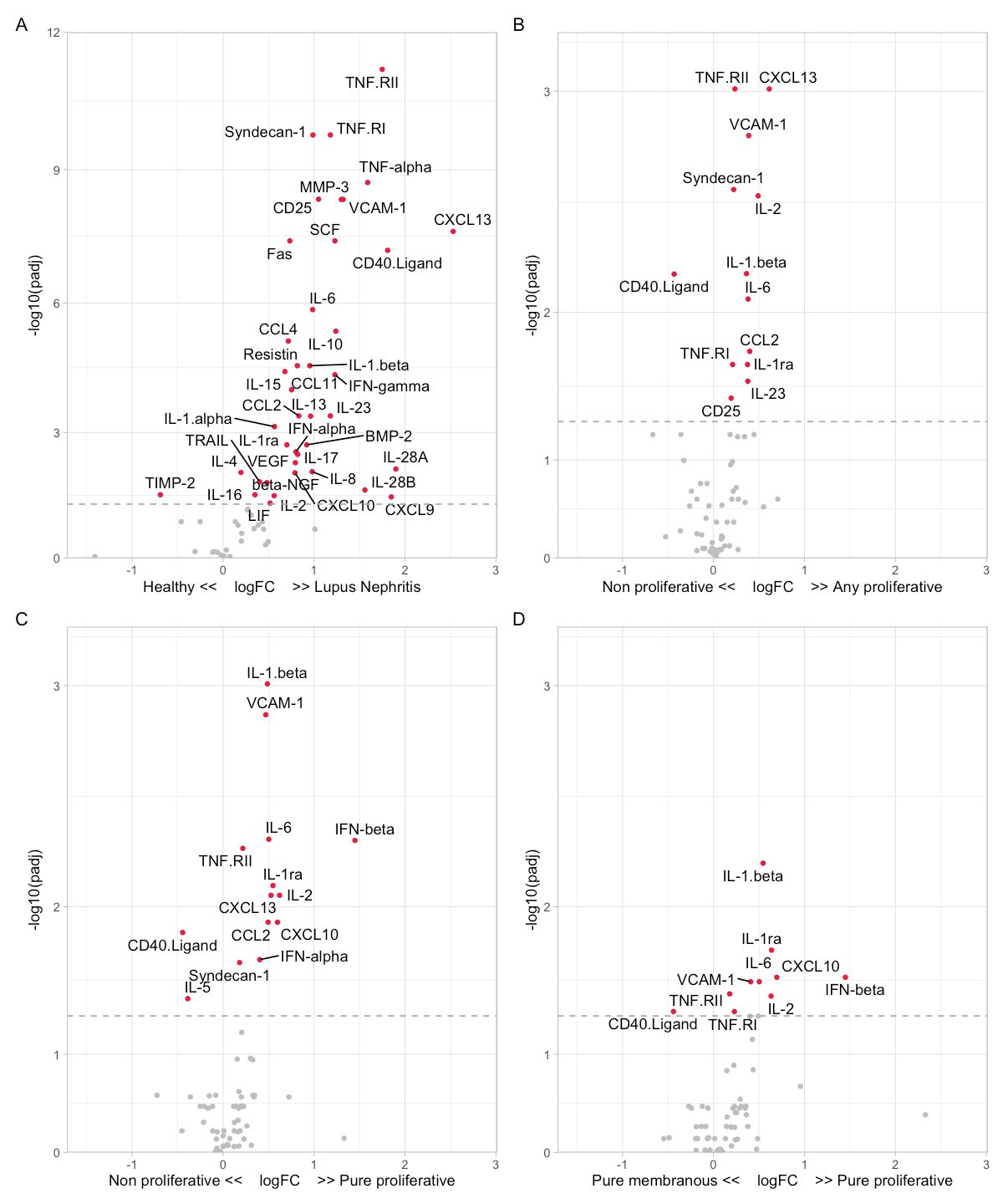
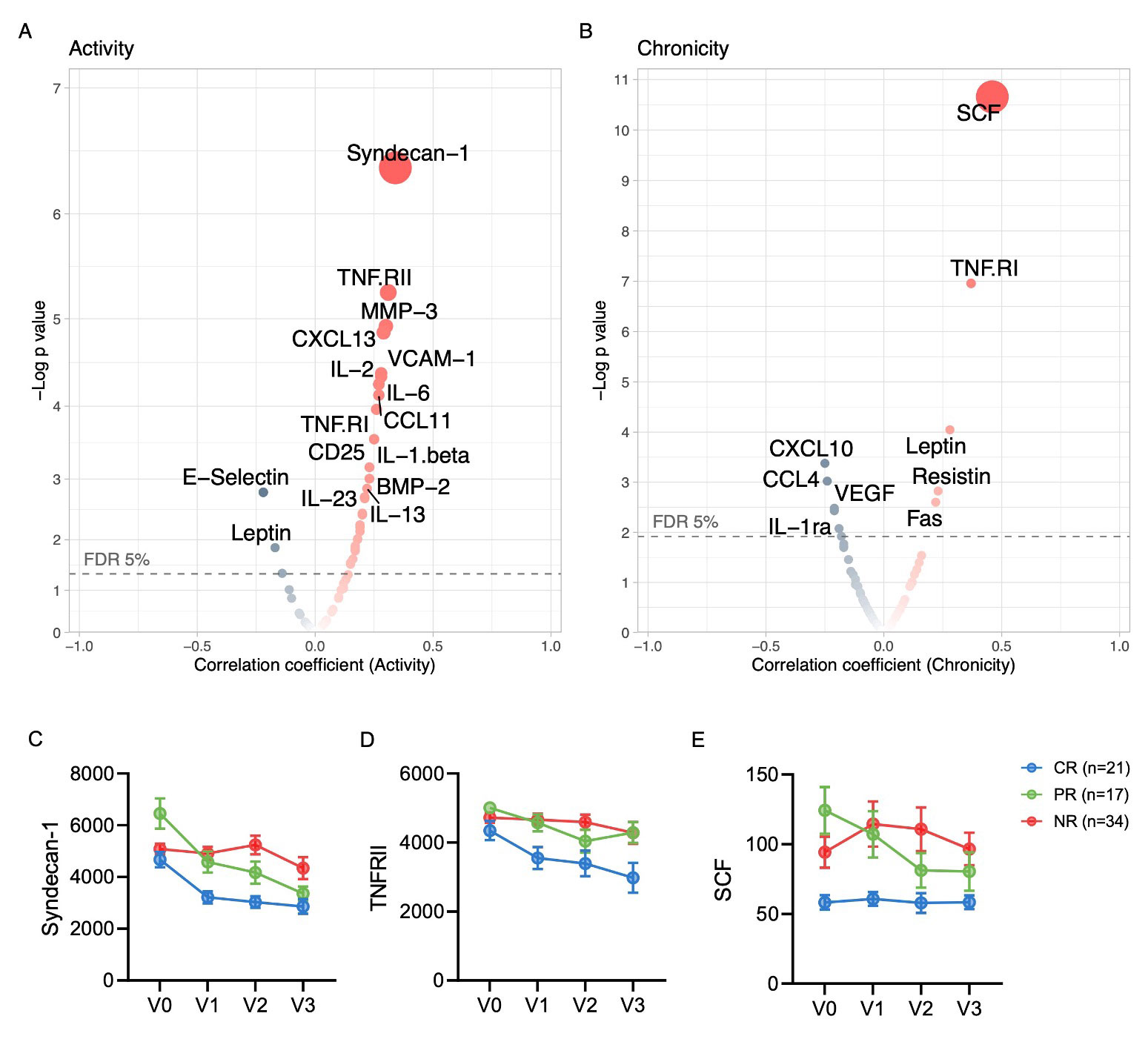
Results: LN patients demonstrated heterogeneity in serum soluble mediator concentrations (Fig 1). Most soluble mediators were elevated in LN patients compared to HD (Fig. 2A). Within LN, patients with proliferative LN (class III +/- V or class IV +/-V) displayed a distinct signature (Fig 2B). In particular, patients with pure proliferative LN (class III or IV) had higher serum levels of immune mediators, such as IFNβ and IL-1β, compared to nonproliferative LN (Fig 2C), including pure membranous (class V) LN (Fig 2D). In addition, several serum immune mediators correlated with intrarenal LN activity (NIH activity index), with syndecan-1 (CD138) and TNF-RII exhibiting the highest correlation (Fig 3A). In contrast, stem cell factor (SCF) and TNF-RI had the highest correlation with the chronicity index (Fig 2B). In proliferative LN, the concentrations of many immune mediators declined in treatment responders (not shown). For example, syndecan-1 and TNF-RII decreased in complete and partial responders but not in nonresponders (Fig 3C-D). In contrast, SCF levels remained relatively stable regardless of response status (Fig 3E).
Conclusion: Distinct histological features of LN are paralleled by specific signatures of circulating soluble mediators. Within LN, proliferative LN is associated with higher circulating levels of inflammatory cytokines, notably, type 1 IFNs. Furthermore, a decline in the titers of several immune mediators correlated with LN activity was associated with treatment response, suggesting a possible role in LN pathogenesis. These signatures and trajectories provide insight into LN pathogenesis, heterogeneity, and biomarker development.
Volcano plots displaying Spearman correlations of the (A) NIH activity index and (B) NIH chronicity index with the serum concentrations of soluble mediators at the time of the diagnostic kidney biopsy. (C-E) Examples of trajectories. Soluble mediator concentrations were measured at the time of kidney biopsy (V0) and 3 (V1), 6 (V2), and 12 (V3) months post-kidney biopsy in patients with proliferative LN (class III +/-V or class IV +/- V). Treatment response was determined at 12 months, with complete response (CR) defined as urine protein//creatinine (UPCR)<0.5, serum creatinine <125% of baseline, and prednisone <10mg/day. Partial response (PR) was defined by the same criteria as CR, except with a UPCR >0.5 with <50% improvement from baseline. Patients who did not meet either requirement were classified as nonresponders (NR).
To cite this abstract in AMA style:
Fava A, Guthridge C, Kheir J, Wagner C, Petri M, Buyon J, Diamond B, (AMP) RA/SLE t, Guthridge J, James J. Serum Soluble Mediator Signatures of Lupus Nephritis Histological Features and Response to Treatment [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/serum-soluble-mediator-signatures-of-lupus-nephritis-histological-features-and-response-to-treatment/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/serum-soluble-mediator-signatures-of-lupus-nephritis-histological-features-and-response-to-treatment/