Session Information
Session Type: Poster Session A
Session Time: 8:30AM-10:30AM
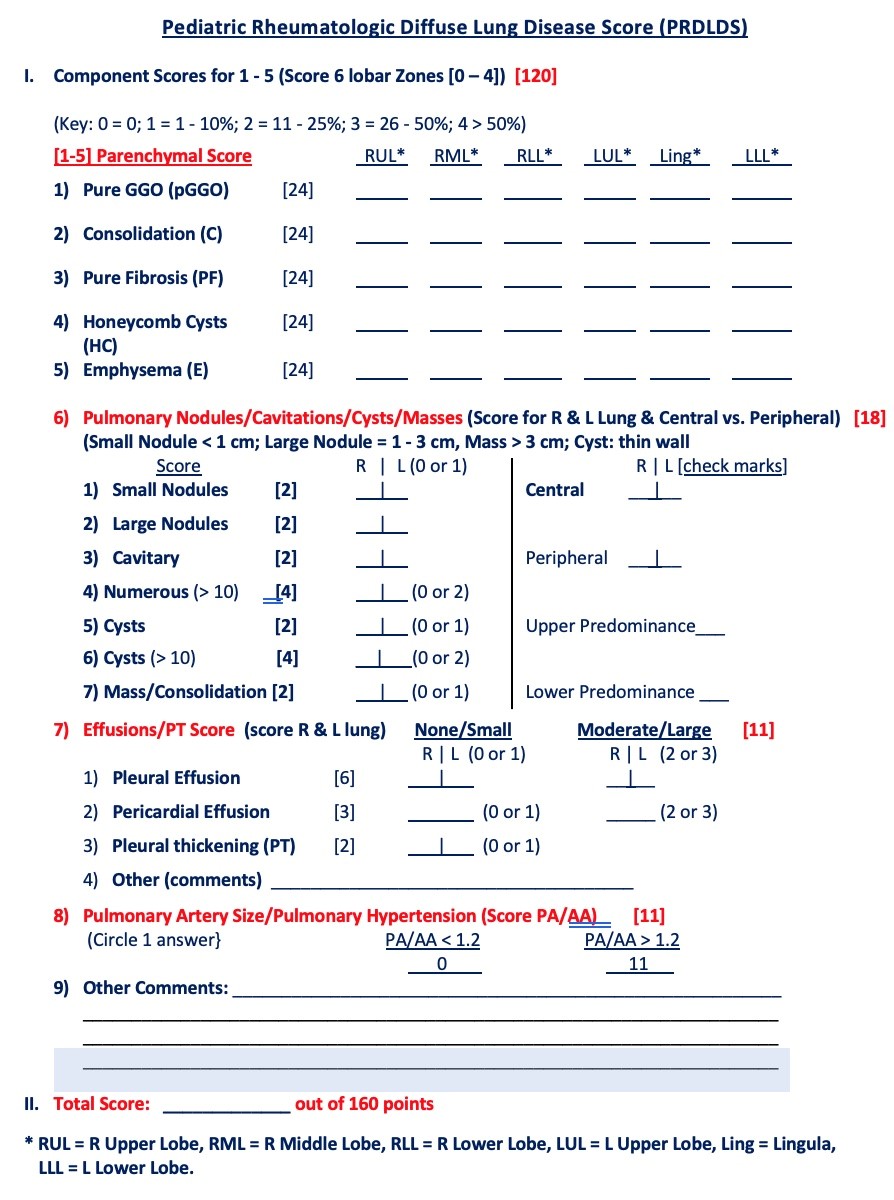
Background/Purpose: Spiral chest CT (SCT) is commonly used to evaluate subclinical lung disease in pediatric rheumatology. However, there are no validated scoring tools to objectively evaluate disease severity. The purpose of this study was to determine the feasibility of a semi-quantitative chest CT scoring system (Pediatric Rheumatologic Diffuse Lung Disease Score [PRDLDS], Table 1) to assess the prevalence of diffuse lung disease (DLD) assessed by SCT in pediatric rheumatologic patients.
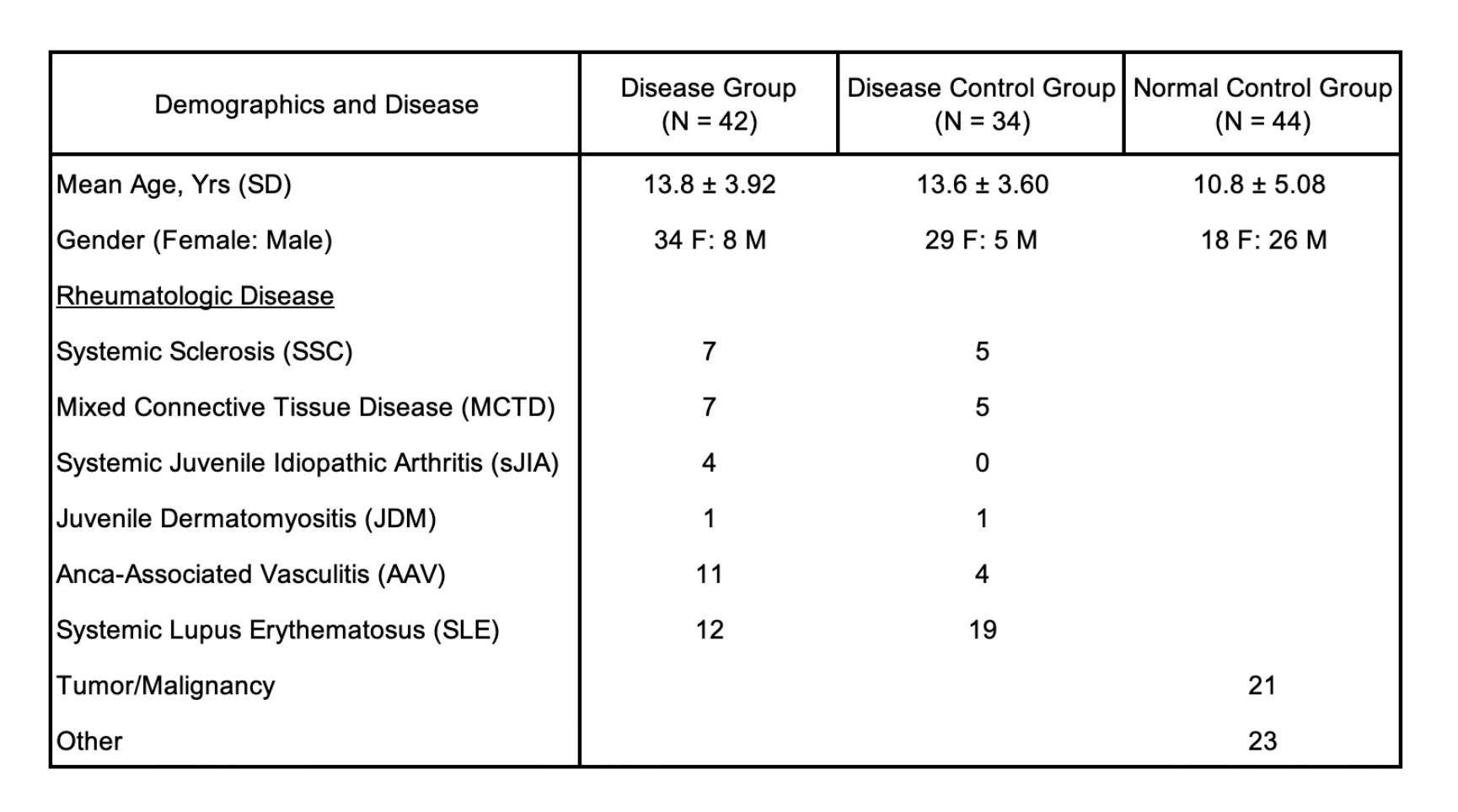
Methods: Three radiologists with varying DLD imaging experience independently scored 1-2 mm inspiratory chest CT scans (96 non-contrast/24 contrast) in 120 pediatric subjects (DG: N=42 PR patients with DLD; DCG: N=34 PR patients without DLD; and NCG: N=44 pediatric normal control subjects with chest CT scans) from 3 medical centers (Children’s Hospital of LA, Stanford Children’s Health, Mayo Clinic). The SCT scoring system was developed as a modification of the Goldin scoring system¹ for systemic sclerosis adults to account for the full spectrum of DLD findings in PR patients (Table 2). It quantifies the extent of disease for 6 lung zones based on 4 domains: 1) parenchymal domain score (PDS); 2) pulmonary nodule/cavitary/cyst/mass DS; 3) total effusion/pleural thickening DS; and 4) pulmonary hypertension domain score (PHDS).
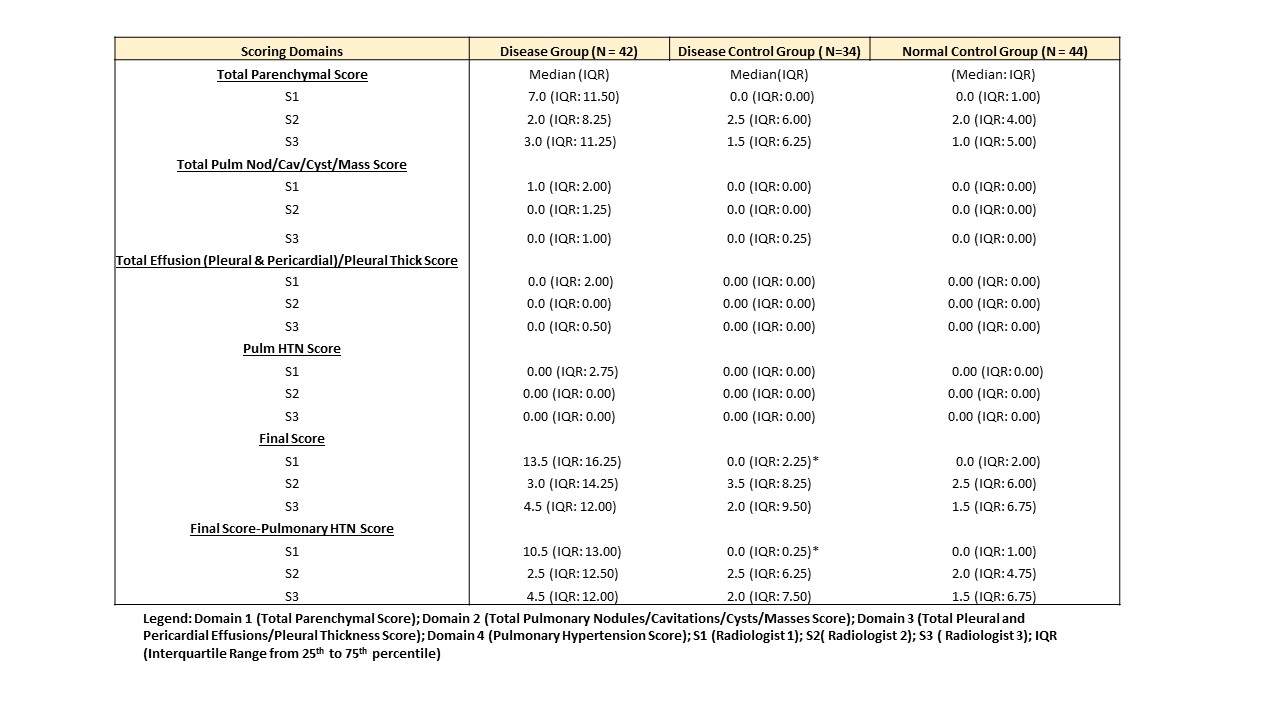
Results: The overall prevalence of DLD in the disease group based on a cutoff score of > 8 for all lung zones was 68% by the most experienced scorer (S1) in comparison to 41% (S2, S3); the prevalence of total disease was primarily driven by the PDS (74% [S1], 38% [S2, S3] with significant contributions from pure ground glass opacities (GGO) and pure fibrosis (PF) subscores (SS). There was lower disease prevalence noted in domains 2 (7 – 19%), 3 (2 – 5%), and 4 (4 – 23%). Prior DLD scoring experience impacted both the PDS and GGO & PF subscores; radiologist (S1) identified more disease and had greater specificity to discriminate between groups than the more naïve DLD scorers; for S1 scorer: DG – PDS (median 7.0 [IQR:11.5]), GGO SS (median 2.5 [IQR: 5.5]), PF SS (median 4.0 [IQR: 5.00] vs. DCG and NCG both having (median 0.0 [IQR:0.0]). Refer to Table 3.
Conclusion: Semi-quantitative scoring using the PRDLDS is a feasible tool to assess DLD in PR patients. Preliminary data revealed that our PR patients had mild DLD which is primarily contributed by parenchymal disease. Our data demonstrated high inter-rater variability for parenchymal scoring, and problems with PHDS which supports that 1) further training with DLD imaging experts is necessary to improve the reliability and validity of the PRDLDS in quantifying milder lung disease ; 2) non-contrast CTs make it more difficult to evaluate PH accurately; 3) quantitative CT assessment tools are needed to reliably evaluate pulmonary interstitial lung disease in pediatric rheumatologic patients. We are currently evaluating our study cohort with CALIPER (Computer Aided Lung Informatics for Pathology Evaluation and Rating), a quantitative chest CT analyzer that is validated in adults with DLD.
Reference:
1. Goldin JG, Lynch DA, Strollo DC, et al. High-resolution CT scan findings in patients with symptomatic scleroderma-related interstitial lung disease. Chest. 2008;134(2):358-367.
To cite this abstract in AMA style:
Cidon M, Robinson T, Newman B, Iskander P, Thacker P, Zucker E, Bartholmai B, Tipre D, Lee T, Pooni R, Moats R. Semi-quantitative Chest Computed Tomography (CT) Analysis in Pediatric Rheumatologic (PR) Patients with Diffuse Lung Disease [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/semi-quantitative-chest-computed-tomography-ct-analysis-in-pediatric-rheumatologic-pr-patients-with-diffuse-lung-disease/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/semi-quantitative-chest-computed-tomography-ct-analysis-in-pediatric-rheumatologic-pr-patients-with-diffuse-lung-disease/