Session Information
Date: Monday, October 27, 2025
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Patients with Sjögren’s Disease (SjD) frequently report debilitating symptoms such as pain, fatigue, and dryness, significantly impacting health-related quality of life. Although sleep disturbances in SjD are well documented, only a few studies have objectively assessed sleep using wrist actigraphy, and none have explored circadian rhythm alterations or their clinical correlates. This study aimed to: (1) evaluate differences in self-reported and actigraphic sleep and circadian parameters between SjD patients and healthy controls (HCs); and (2) examine associations between these disruptions and clinical indices, including disease activity and patient-reported outcomes.
Methods: In this cross-sectional study, we enrolled female SjD patients meeting the 2016 ACR/EULAR criteria, along with age-, sex-, and BMI-matched HCs. Participants underwent 7-day wrist actigraphy. Subjective measures included the Pittsburgh Sleep Quality Index (PSQI), Epworth Sleepiness Scale (ESS), and reduced Morningness-Eveningness Questionnaire (rMEQ). Circadian rhythm parameters were estimated using both parametric and non-parametric methods. Patient-reported outcomes included the EULAR Sjögren’s Syndrome Patient Reported Index (ESSPRI), Functional Assessment of Chronic Illness Therapy (FACIT), and Hospital Anxiety and Depression Scale (HADS). Disease activity was assessed using the EULAR Sjögren’s Syndrome Disease Activity Index (ESSDAI).
Results: Forty-six SjD patients and forty HCs were included. Compared to controls, SjD patients reported poorer sleep quality (higher PSQI scores) and greater daytime sleepiness (higher ESS). Actigraphy revealed lower sleep efficiency (SE), increased wake after sleep onset (WASO), an earlier sleep midpoint, and a significantly advanced sleep midpoint and acrophase, indicating an objective shift towards eveningness (Table 1, Fig 1). Higher ESSPRI and HADS scores were associated with worse subjective sleep quality, greater sleepiness, lower total sleep time, reduced sleep efficiency, and increased WASO. Higher ESSDAI scores correlated with reduced daytime activity levels (lower MESOR) and fewer daily steps. Sensitivity analyses suggested that greater disease activity was linked to longer total sleep time and reduced sleep regularity (Table 2).
Conclusion: Conclusions: SjD is associated with both subjective and objective disruptions in sleep and circadian rhythms. These alterations correlate with disease activity and patient-reported outcomes, especially fatigue, mood disturbances, and physical inactivity. Circadian rhythm dysregulation may represent an underrecognized aspect of SjD, with potential implications for future therapeutic approaches.
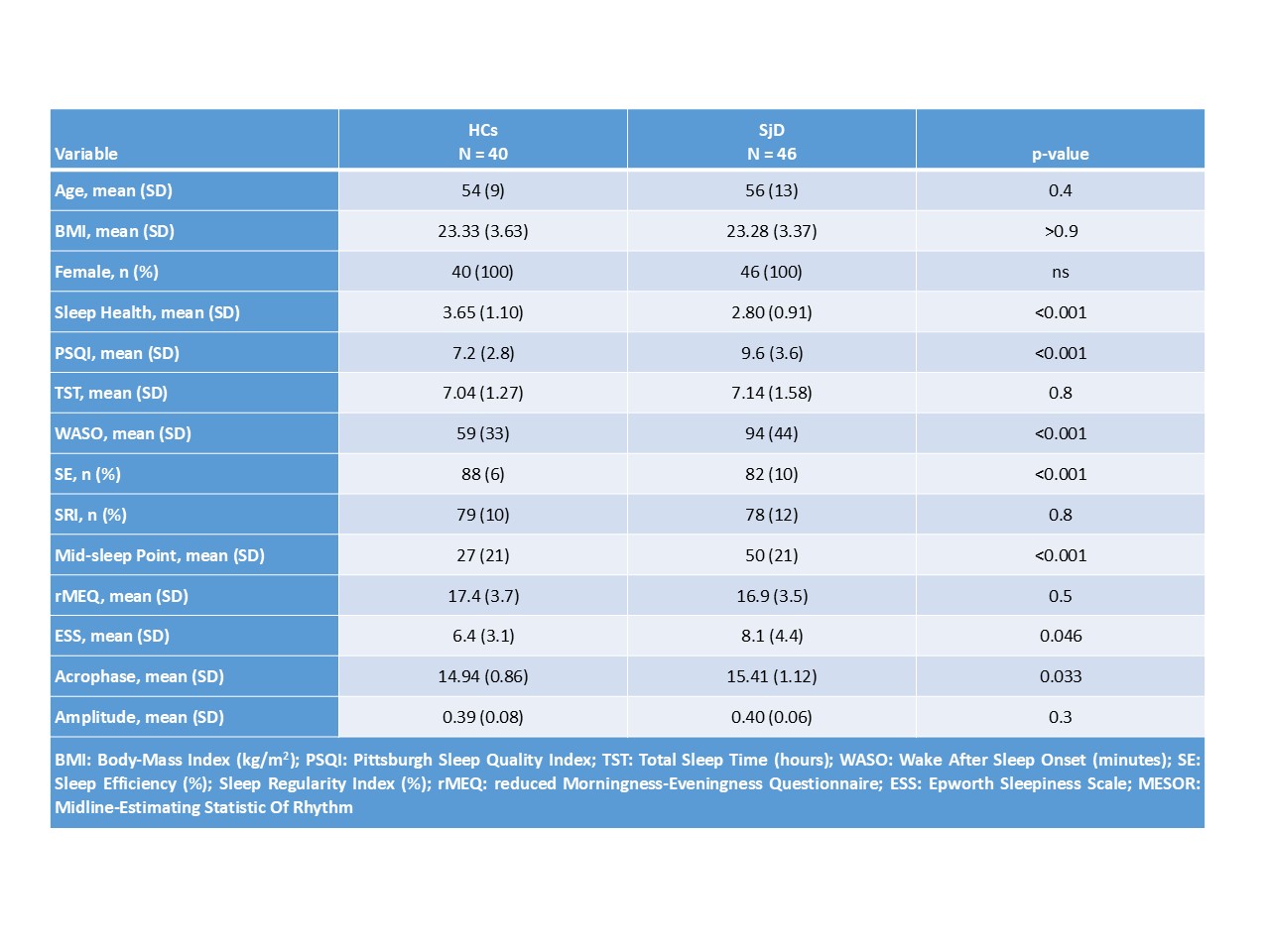 Table 1: Self-reported and Actigraphic Sleep and Circadian Rhythm Parameters in SjD and HCs
Table 1: Self-reported and Actigraphic Sleep and Circadian Rhythm Parameters in SjD and HCs
.jpg) Fig.1 F-Test for 24h-circadian activity
Fig.1 F-Test for 24h-circadian activity
.jpg) Table 2: Multiple Linear Regression Models Exploring Associations Between ESSPRI, HADS, and Sleep–Circadian Parameters
Table 2: Multiple Linear Regression Models Exploring Associations Between ESSPRI, HADS, and Sleep–Circadian Parameters
To cite this abstract in AMA style:
Di Pede C, Colitta A, Di Galante M, Bruno S, Donati S, Dei B, Fulvio G, La Rocca G, Talarico R, Mosca M, Baldini C, Faraguna U. Self-Reported and Actigraphic Sleep and Circadian Rhythm Disruptions in Patients with Sjögren’s Disease: Associations with Disease Activity and Patient-Reported Outcomes [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/self-reported-and-actigraphic-sleep-and-circadian-rhythm-disruptions-in-patients-with-sjogrens-disease-associations-with-disease-activity-and-patient-reported-outcomes/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/self-reported-and-actigraphic-sleep-and-circadian-rhythm-disruptions-in-patients-with-sjogrens-disease-associations-with-disease-activity-and-patient-reported-outcomes/
