Session Information
Date: Sunday, November 13, 2022
Title: Spondyloarthritis Including PsA – Diagnosis, Manifestations, and Outcomes Poster III
Session Type: Poster Session C
Session Time: 1:00PM-3:00PM
Background/Purpose: Lack of timely rheumatology referral for suspected axial spondyloarthritis (axSpA) is a major contributor to delayed diagnosis in patients with chronic back pain (CBP). Poor disease awareness among non-rheumatologists and busy practice patterns adversely affect referral process. In this study we evaluated the effectiveness of a self-referral strategy using an online screening tool distributed to at risk patients using electronic medical record and social media.
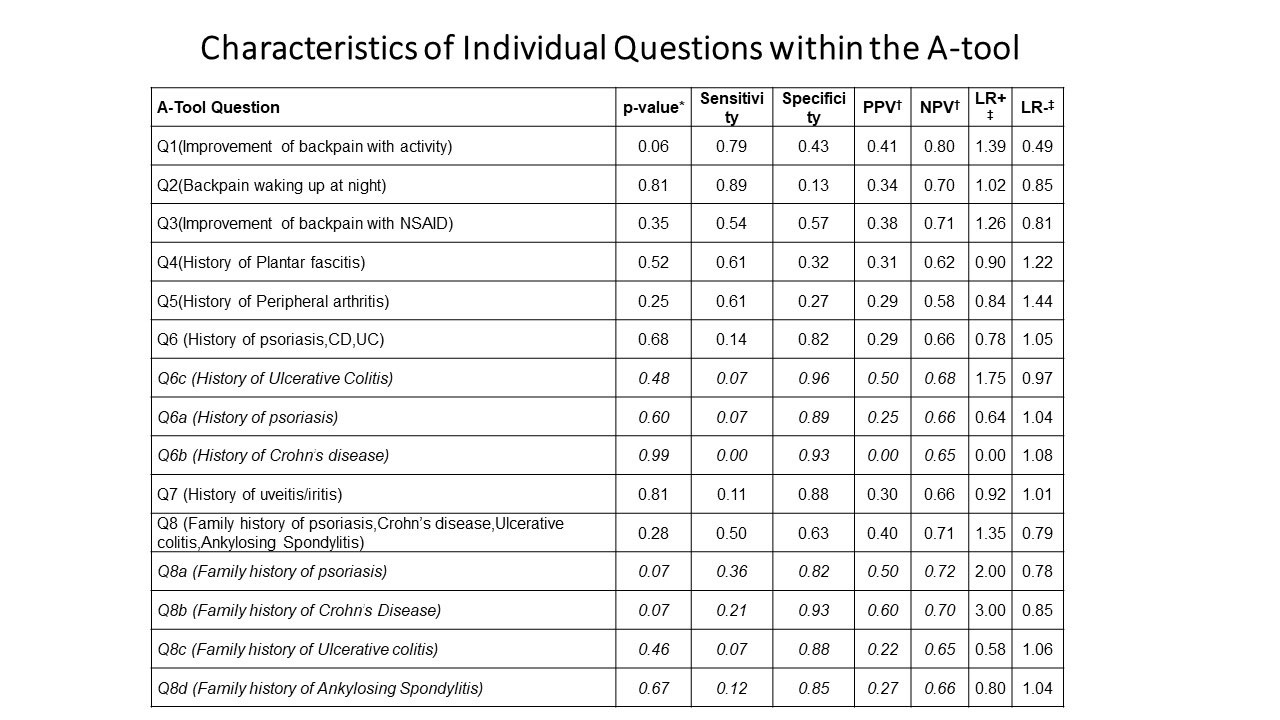
Methods: Based on the predictive values of spondyloarthritis features, we developed a screening tool (A-tool) consisting of a 3 question prescreen and 8 question screening questionnaire (SQ). A-tool was distributed via patient portal (Mychart) to patients age 18 to 65 years who had CBP listed as a medical problem in their electronic medical record and also via Facebook to general population in our geographical area. Patients who passed all 3 questions in pre-screen could access the SQ and those with 3 or more positive responses on SQ were invited for study visit after confirming the eligibility. Patients with known diagnosis of axSpA, age >65 yr and previous spine surgery were excluded. Patients underwent history and physical, labs (CRP and HLA-B27) and imaging studies (X-ray and MRI of pelvis). Clinician’s judgement was considered gold standard for diagnosis of axSpA. DNA and plasma samples have been stored for biomarker research. Statistical analysis was done with descriptive statistics, logistic regression, T-test and chi-square tests.
Results: Total 1289 patients took the survey through MyChart (51%) or Facebook (49%) from April 2019 to February 2022 (Table 1). Among the responders, 851 (66%) had positive pre-screen and 653 (51%) had positive A-tool. As of May 2022, 100 patients were enrolled of which 84 patients completed a study visit, labs and imaging. Remaining 16 did not complete labs or imaging studies after the study visit. Out of 84 patients, 28 (33%) were diagnosed with axSpA. There were 7 patients with AS and 21 with nr-axSpA. Predictive values of individual questions in the A-tool are described in Table 3. Further analysis of data is underway.
Conclusion: Our findings suggest that A-tool based self-referral strategy for early diagnosis of axSpA among patients with CBP is practical and feasible approach. Combination of SpA features may be more useful for referral as compared to individual features. We need larger prospective study to validate our findings.
To cite this abstract in AMA style:
Danve A. Self-referral Strategy for Early Diagnosis of Axial Spondyloarthritis- Preliminary Analysis from Finding Axial Spondyloarthritis Study [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/self-referral-strategy-for-early-diagnosis-of-axial-spondyloarthritis-preliminary-analysis-from-finding-axial-spondyloarthritis-study-2/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/self-referral-strategy-for-early-diagnosis-of-axial-spondyloarthritis-preliminary-analysis-from-finding-axial-spondyloarthritis-study-2/