Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Mycophenolate mofetil (MMF) is commonly used to treat major SLE manifestations; however, it is associated with significant toxicities. Thus, MMF withdrawal is desirable in patients after achieving remission. This study investigates baseline immune cell populations as potential predictors of flare risk after MMF cessation, aiming to optimize MMF therapy.
Methods: We recruited 102 SLE patients with quiescent SLE (clinical SLEDAI< 4) on long-term MMF and baseline hydroxychloroquine as part of the “Randomized MMF Withdrawal in Systemic Lupus Erythematosus (SLE) (ALE06)” Autoimmune Center of Excellence Network trial (Chakravarty, et al. Lancet Rheum. 2024). Patients were randomly assigned to continue (n=50) or withdraw MMF over 12 weeks (n=52). Flares were determined over 60 weeks using the Safety of Estrogens in Lupus Erythematosus National Assessment-SLEDAI. Blood was collected, and PBMCs were isolated at baseline for immunophenotyping via 43-parameter cytometry by time-of-flight (CyTOF).
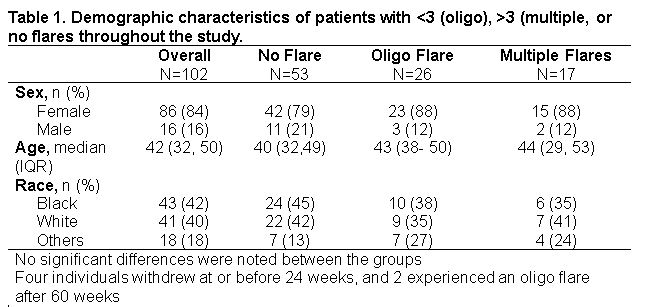
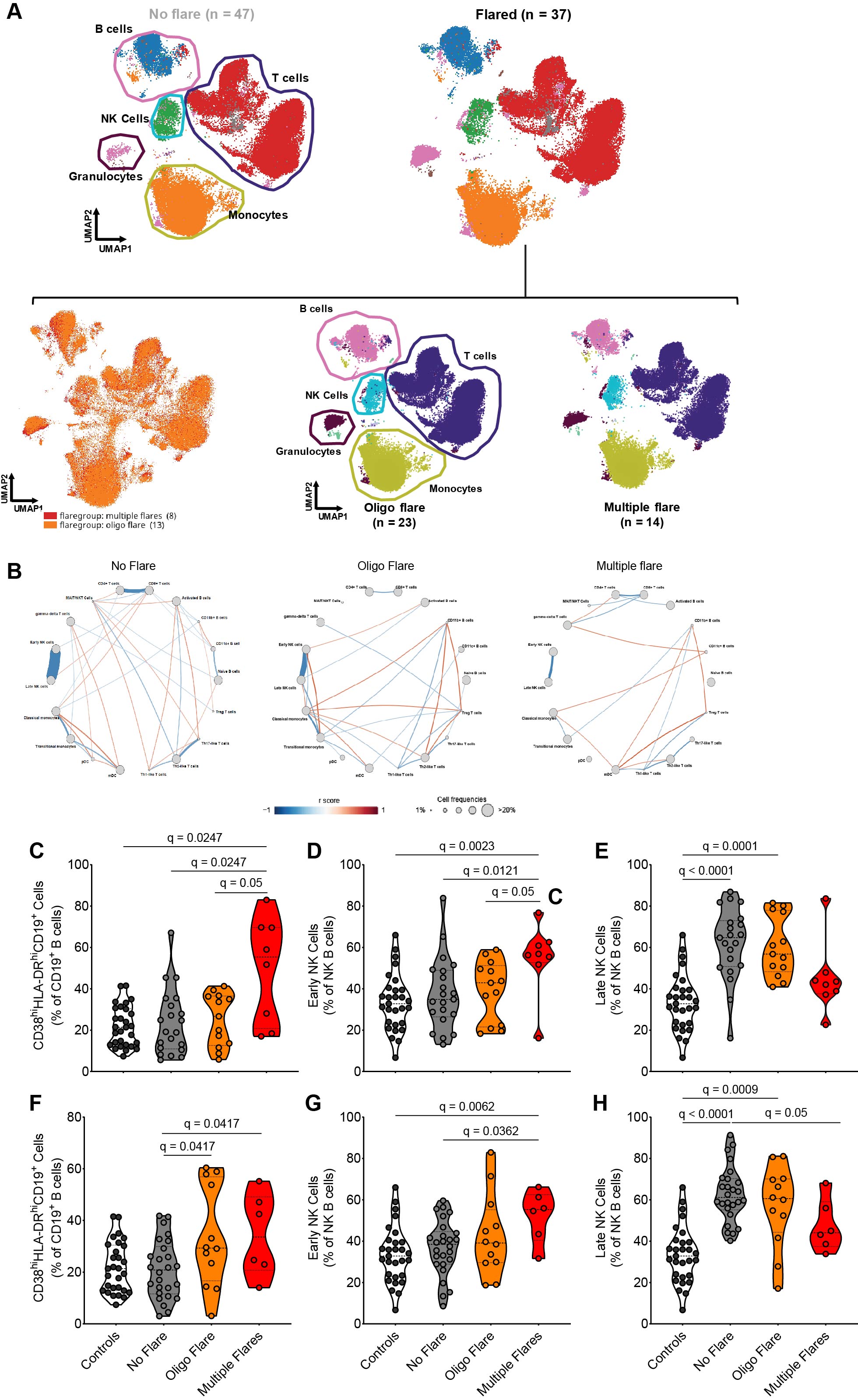
Results: Over 60 weeks, 53 patients had no flares, 28 had < 3 flares (oligo flare), 17 patients had >3 flares (multiple flares), and 4 withdrew from the study. There was no significant difference in sex, age, or race in the patients with or without flares (Table 1). At baseline, the immune phenotype was altered in patients who experienced oligo or multiple flares (Figure 1A). Furthermore, a correlation network analysis showed that there were fewer inter-cellular connections among different immune cells in patients who experienced flares compared to those without flares, with even fewer in those with multiple flares, supporting a more dysregulated immune system in patients with impending flare (Figure 1B). In particular, patients with multiple flares post-MMF withdrawal exhibited a significantly higher baseline frequency of activated B cells and early NK cells and a lower frequency of late NK cells compared to controls and patients with oligo or no flares (Figure 1C-E). Similar findings occurred in patients who maintained MMF (Figure 1F-H). Finally, a Random Forest machine-learning model based on the baseline frequencies of activated B cells and early and late NK cells had ~72 and 76.0% accuracy for predicting patients who will ultimately experience any flare or multiple flares after withdrawing MMF, respectively.
Conclusion: Patients exhibit immune cell dysregulation, characterized by elevated frequencies of activated B cells and early NK cells and reduced frequencies of late NK cells, prior to experiencing flares, regardless of maintaining or withdrawing MMF therapy. Importantly, models encompassing these cell subsets may predict which patients will flare upon withdrawing MMF, highlighting the potential to identify large subsets of quiescent lupus patients who can safely withdraw therapy.
NIAID/NIH Autoimmunity Centers of Excellence Award (U19AI110483; IS)
To cite this abstract in AMA style:
Wright C, Lu R, Wagner C, Guthridge C, Macwana S, Chakravarty E, Utset T, Kamen D, Contreras Martin G, McCune W, Aranow C, Kalunian K, Massarotti E, Clowse M, Rovin B, Lim S, Majithia V, Looney R, Dall'Era M, Erkan D, Saxena A, Olsen N, Ko K, Goldmuntz E, Barry W, Pinckney A, Clinical Study Team A, James J, Guthridge J. Select Immune Cell Dysregulation Identifies Clinically Quiescent Patients at Risk of Flare Who Stop Mycophenolate Mofetil While Continuing Hydroxychloroquine [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/select-immune-cell-dysregulation-identifies-clinically-quiescent-patients-at-risk-of-flare-who-stop-mycophenolate-mofetil-while-continuing-hydroxychloroquine/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/select-immune-cell-dysregulation-identifies-clinically-quiescent-patients-at-risk-of-flare-who-stop-mycophenolate-mofetil-while-continuing-hydroxychloroquine/