Session Information
Date: Tuesday, November 9, 2021
Title: Spondyloarthritis Including PsA – Treatment Poster III: Psoriatic Arthritis II (1801–1835)
Session Type: Poster Session D
Session Time: 8:30AM-10:30AM
Background/Purpose: Psoriasis (PsO), Psoriatic Arthritis (PsA) and Axial Spondyloarthritis (AxSpA) are chronic immune-mediated inflammatory diseases (IMIDs) requiring long-term treatment. Systemic inflammation in these IMIDs is associated with cardiovascular (CV) disease1,2. High sensitivity C-reactive protein (hsCRP) is an independent surrogate CV risk marker. Recently, high neutrophil-lymphocyte ratio (NLR) has emerged as a novel inflammatory biomarker predictive of CV disease and overall mortality3. Here, we report the effect of IL-17A inhibition with secukinumab on CV risk parameters in PsO, PsA and AxSpA patients over 1 year of treatment.
Methods: This is a post-hoc analysis of pooled Phase 3/4 secukinumab studies in PsO, PsA and AxSpA. CV-related exclusion criteria included uncontrolled hypertension and congestive heart failure. Traditional (body mass index [BMI], fasting glucose, blood pressure, cholesterol and lipids) and inflammatory CV risk parameters (hsCRP, absolute neutrophil count and NLR) were assessed. Exploratory statistical comparison of median change from baseline to Week 12 (PsO) or Week 16 (PsA/AxSpA) for secukinumab vs placebo was performed by Wilcoxon 2-sample test. Subgroup analyses were performed in high-risk patients (baseline hsCRP >10 mg/L in PsA/AxSPA and >4 mg/L in PsO).
Results: In total, 9,197 patients from 19 clinical trials (8 in PsO, n=4,742; 5 in PsA, n=2,475; 6 in AxSpA, n=1,980) were included. All traditional CV risk parameters remained stable in secukinumab-treated patients through 1 year (Table 1). Secukinumab administration rapidly reduced both hsCRP and the NLR, compared with placebo at Week 12 (PsO) or Week 16 (PsA/AxSPA) in the overall population and in high-risk patients defined by having high baseline hsCRP (all p< 0.01). This reduction was maintained for at least 1 year of secukinumab therapy in all indications (Table 2). In some patients where available follow-up data allowed exploratory analysis through five years, secukinumab induced sustained reductions in hsCRP and NLR; traditional CV risk factors did not change.
Conclusion: Secukinumab rapidly reduced hsCRP and the NLR in patients with IMIDs with a high systemic inflammatory burden. Traditional CV risk factors remained stable for at least 1 year in patients with PsO, PsA and AxSpA.
References:
1. Papagoras, et al. Joint Bone Spine. 2014;81:57‒63.
2. Aksentijevich, et al. Trends Cardiovasc Med. 2020;30:472-8.
3. Kim, et al. JAMA Cardiol. 2018;3:455-62.
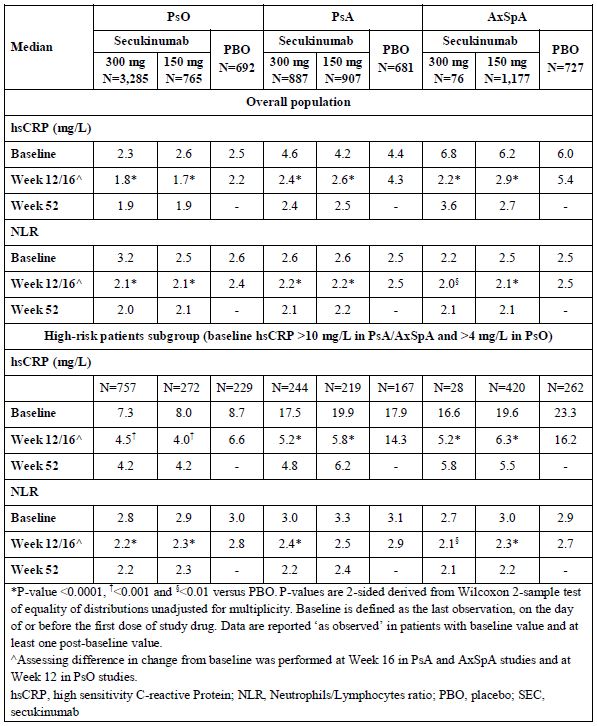 Table 1. Inflammatory Risk Parameters: Weeks 12/16 and 52
Table 1. Inflammatory Risk Parameters: Weeks 12/16 and 52
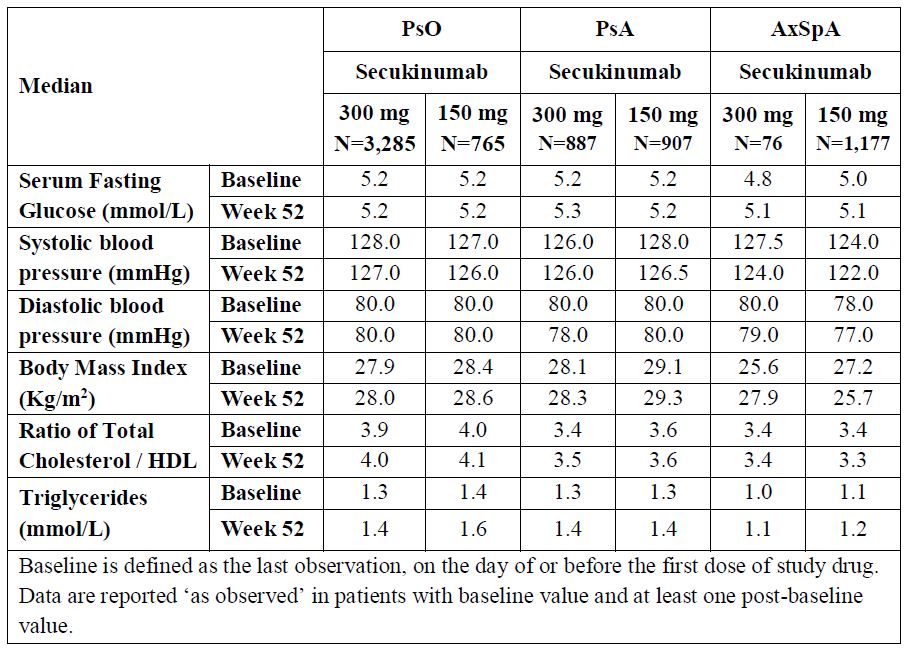 Table 2. Traditional CV Risk Factors: Week 52
Table 2. Traditional CV Risk Factors: Week 52
To cite this abstract in AMA style:
Merola J, McInnes I, Deodhar A, Quebe-Fehling E, Aassi M, Peine M, Mehta N. Secukinumab Effects on Cardiometabolic Risk and Systemic Inflammation in Patients with Psoriasis, Psoriatic Arthritis and Axial Spondyloarthritis: Results from Post Hoc Analyses of Pooled Data from 19 Phase 3/4 Clinical Studies [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/secukinumab-effects-on-cardiometabolic-risk-and-systemic-inflammation-in-patients-with-psoriasis-psoriatic-arthritis-and-axial-spondyloarthritis-results-from-post-hoc-analyses-of-pooled-data-from-19/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/secukinumab-effects-on-cardiometabolic-risk-and-systemic-inflammation-in-patients-with-psoriasis-psoriatic-arthritis-and-axial-spondyloarthritis-results-from-post-hoc-analyses-of-pooled-data-from-19/
