Session Information
Date: Tuesday, November 14, 2023
Title: (1913–1944) Miscellaneous Rheumatic & Inflammatory Diseases Poster III
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Scleritis involves inflammation of the sclera caused by trauma, infections, or autoimmune conditions. The purpose of our study was to understand the relationship between scleritis and the presence of autoimmune disease, including the temporal relationship, treatment course, recurrence, and associated serologies.Characterizing the relationship between scleritis and autoimmunity can help clinicians identify and treat conditions effectively.
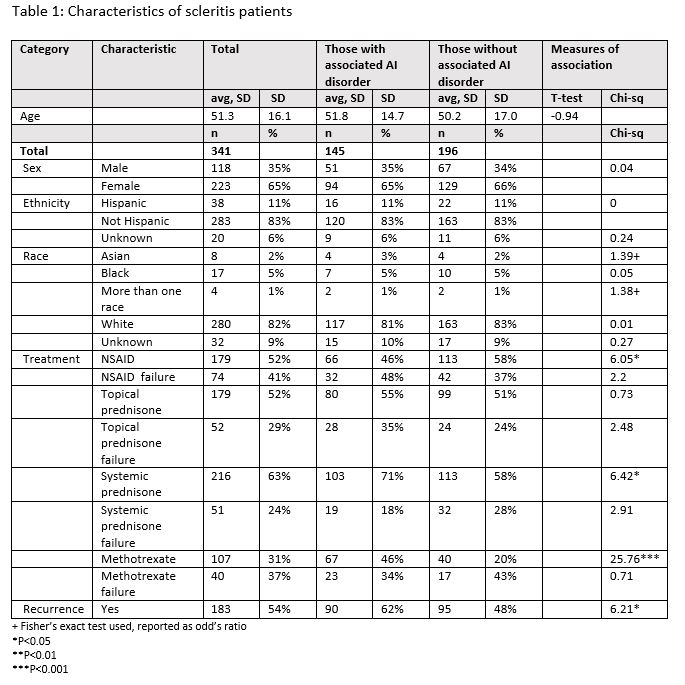
Methods: We conducted a case series of 341 scleritis patients seen between January 1, 2005 and December 20, 2020. Demographics, treatment types, treatment failures, recurrence events, and serology data were compared among patients with and without autoimmune disorders. Autoimmune disorders were described by disease and by time course. American College of Rheumatology criteria were unable to be used to verify diagnoses for this study.
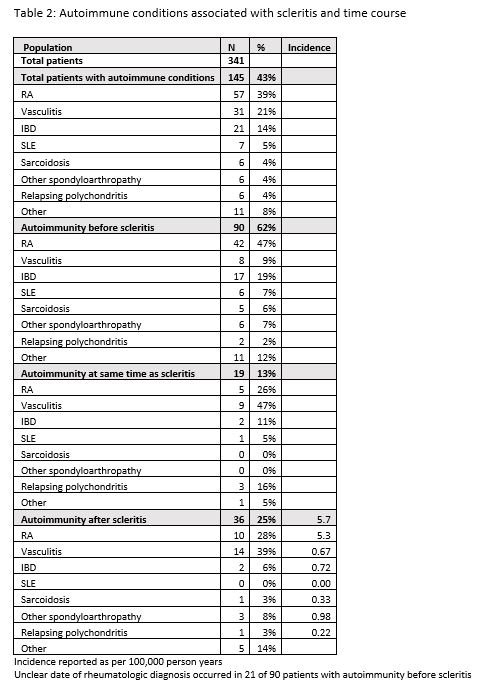
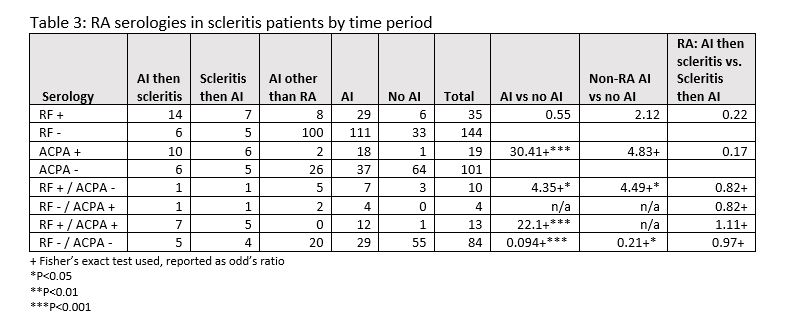
Results: Most patients with scleritis had an associated autoimmune disorder (n=196, 57%), and most patients developed their disorder before scleritis (62%). There were no significant differences in age, gender, ethnicity, or race among scleritis patients with and without autoimmune disorders. Most patients had recurrence of scleritis (54%), and patients with autoimmune disorders were more likely to have a recurrence (62% vs 48%, p< 0.05). The most common scleritis treatments were nonsteroidal anti-inflammatory drugs, topical and systemic prednisone. There were no differences in treatment failure rates based on having an autoimmune disorder. The most common autoimmune disorders associated with scleritis were rheumatoid arthritis (39%), vasculitis (21%), and inflammatory bowel disease (14%). The incidence of autoimmune disorders developed after scleritis for any condition was 0.84/100,000 person years, with 0.33/100,000 person years for vasculitis, and 0.23/100,000 person years for RA. Based on limited data, there were no relationships between RF and ACPA serologies and time course of developing autoimmune disorders and scleritis. Dual-seropositive patients were more likely to have an autoimmune disorder compared to seronegative patients (72% vs 35%, p< 0.001), as were RF+/ACPA- patients (70% vs 35%,p< 0.05).
Conclusion: Scleritis is associated with autoimmune diseases, most commonly developed before scleritis. Scleritis among autoimmune patients is more likely to recur. Comparative studies are needed to identify individual risk factors associated with development of autoimmune disease among scleritis patients.
To cite this abstract in AMA style:
Morrison T, Gottman M, Friedman M, Ghetie D. Scleritis and Development of Autoimmune Disease: A Case Series [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/scleritis-and-development-of-autoimmune-disease-a-case-series/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/scleritis-and-development-of-autoimmune-disease-a-case-series/