Session Information
Session Type: Abstract Session
Session Time: 10:15AM-10:30AM
Background/Purpose: RA-associated lung disease (RA-LD), including RA-associated interstitial lung disease (RA-ILD) and RA-associated bronchiectasis (RA-BR), contributes significantly to morbidity and mortality in RA patients. RA is associated with a 2-fold increased risk of serious infection compared to the general population. However, the association of RA-LD and the risk of serious infection is unclear.
Methods: We conducted a retrospective matched cohort study of patients enrolled in the biobank of a large U.S. health care system, comparing RA-LD cases to RA patients without lung disease (RA-no LD), matched by calendar date, age, sex, and RA duration at the index date of RA-LD diagnosis. Patients with RA met the 2010 ACR/EULAR classification criteria. RA-LD cases were verified by medical record review and chest imaging for clinically-apparent RA-ILD and/or RA-BR. The primary outcome was serious infection, defined as infections requiring hospitalization. Secondary outcomes included any infection, infections by anatomic site, pathogen type, and specific pathogens. Incidence rates and propensity score-adjusted subdistribution hazard ratios (sdHR) using Fine and Gray models to account for competing risk of death were calculated for RA-LD vs. RA-no LD as well as RA-ILD or RA-BR vs. RA-no LD.
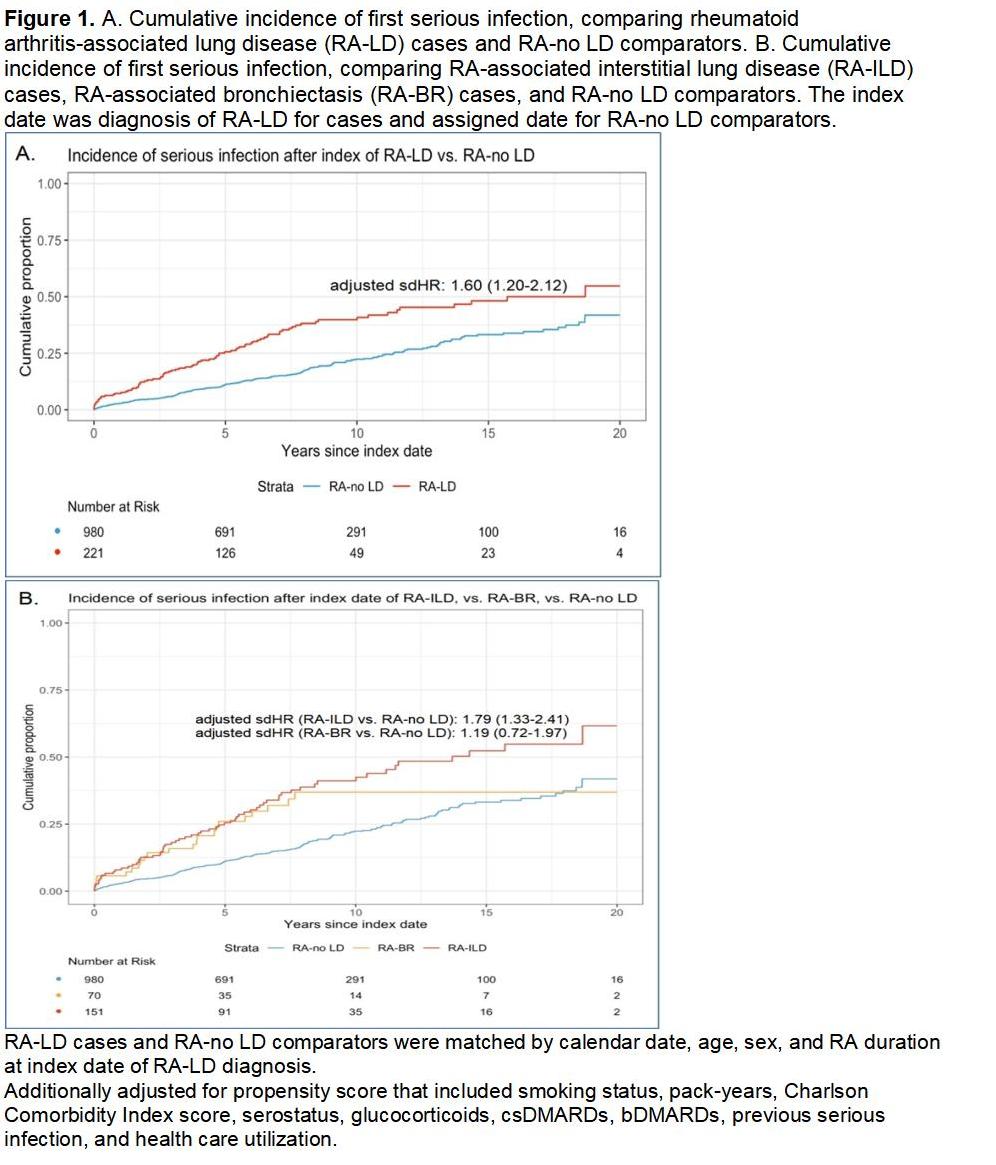
Results: We analyzed 221 RA-LD cases (151 RA-ILD and 70 RA-BR) and 980 RA-no LD matched comparators. After propensity score adjustment, RA-LD cases had a significantly higher risk of serious infections compared to RA-no LD comparators (55.8 vs. 25.8 per 1,000 person-years, adjusted sdHR 1.60, 95%CI 1.20-2.12, Figure 1). The increased risk remained significant for RA-ILD cases (adjusted sdHR 1.79, 95%CI 1.33-2.41), but not for RA-BR cases (adjusted sdHR 1.19, 95%CI 0.72-1.97). Anatomic sites of infection that were more common in RA-LD cases vs. RA-no LD comparators, including pulmonary (31% vs. 10%, p< 0.001), skin and soft tissue (13% vs. 7%, p=0.006), and ear, nose and throat (7% vs. 2%, p=0.002, Table 1). RA-LD was associated with pathogen types: viral (16% vs. 8%, p< 0.001), bacterial (19% vs. 9%, p< 0.001), fungal (10% vs. 3%, p< 0.001), and mycobacterial infections (2% vs. 0.1%, p=0.001). Specific pathogens with higher frequency in RA-LD cases vs. RA-no LD comparators, particularly among RA-BR cases, included influenza virus (7% vs. 2%, p=0.008), respiratory syncytial virus (3% vs. 0.3%, p=0.04), Staphylococcus (14% vs. 6%, p=0.005), Pseudomonas (10% vs. 1%, p< 0.001), and nontuberculous mycobacteria (11% vs. 0.7%, p< 0.001, Table 2).
Conclusion: RA-LD, particularly RA-ILD, was associated with higher risk of serious infection across anatomic sites and diverse pathogen types. While RA-BR was not associated with serious infection, it was associated with higher risk of pulmonary infection and nontuberculous mycobacterial infection. Findings may be explained by lung damage and/or more intense immunosuppression, so tailored infection prevention strategies, including vaccination, are essential for this vulnerable population.
To cite this abstract in AMA style:
ZHANG Q, Qi Y, Wang X, McDermott G, Chang S, Chaballa M, Khaychuk V, Paudel M, Sparks J. Risk of serious infection in patients with rheumatoid arthritis-associated interstitial lung disease or bronchiectasis: A matched cohort study [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/risk-of-serious-infection-in-patients-with-rheumatoid-arthritis-associated-interstitial-lung-disease-or-bronchiectasis-a-matched-cohort-study/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/risk-of-serious-infection-in-patients-with-rheumatoid-arthritis-associated-interstitial-lung-disease-or-bronchiectasis-a-matched-cohort-study/

.jpg)
.jpg)