Session Information
Date: Monday, November 8, 2021
Title: Osteoporosis & Metabolic Bone Disease – Basic & Clinical Science Poster (1135–1149)
Session Type: Poster Session C
Session Time: 8:30AM-10:30AM
Background/Purpose: Patients with systemic sclerosis (SSc) are at high risk for osteoporosis (OPO) and fragility fractures, although their exact prevalences are unknown. This might be due to traditional risk factors for OPO, such as previous fragility fractures, low BMI, use of glucocorticoids. However, the impact of SSc disease-specific characteristics remains unclear. The aim of this study was to estimate the prevalence of OPO and fragility fractures in a large cohort of SSc patients and to identify risk factors.
Methods: We performed a cross-sectional study involving patients fulfilling ACR/EULAR 2013 SSc classification criteria followed prospectively in two European university hospital cohorts between 2004 and 2020. We used databases prospectively collecting SSc related variables including clinical phenotype, organ involvement, autoantibodies, pulmonary function tests, and biological parameters. Bone health parameters were added retrospectively including bone densitometry (DXA), history of fragility fractures and anti-osteoporotic treatment. OPO was defined by a femoral or lumbar spine T-score below -2.5 and/or history of main osteoporotic fracture and/or prescription of anti-osteoporotic drugs.
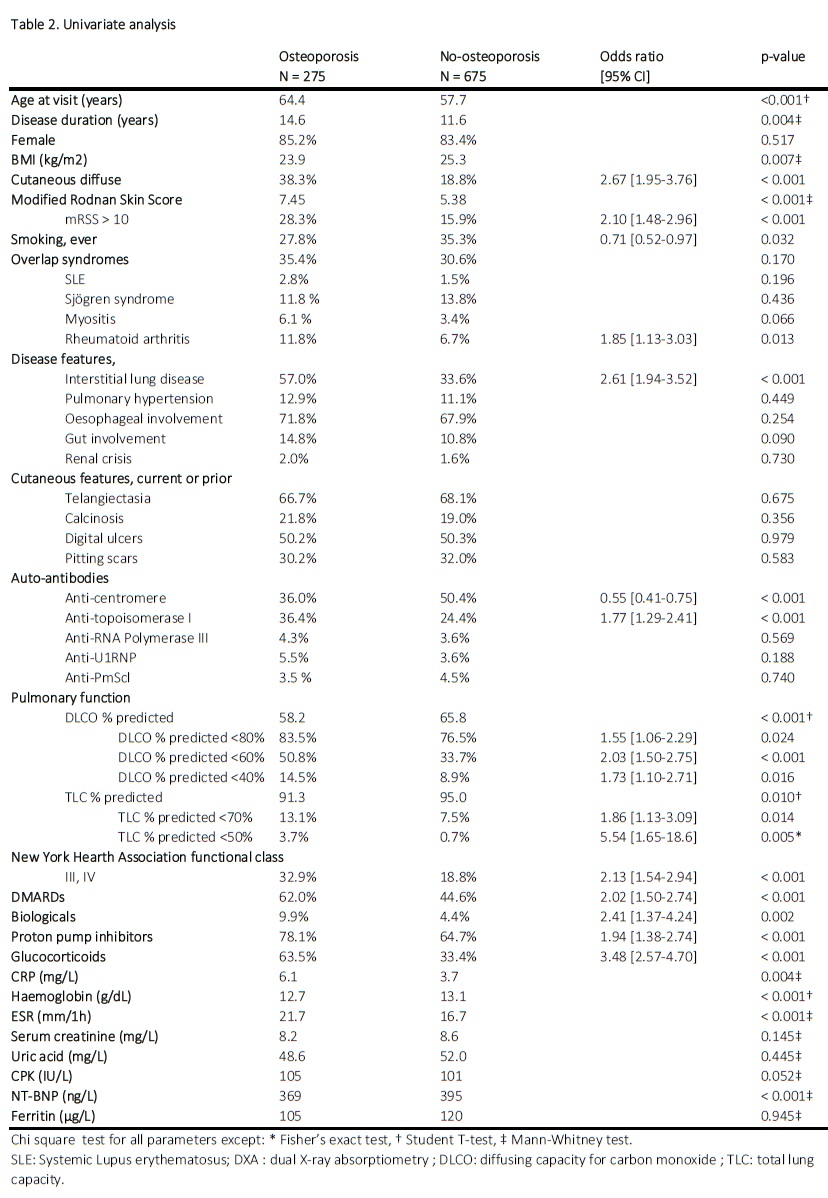
Parametric and non-parametric tests were used to compare osteoporotic and non-osteoporotic patients. Odds ratios were calculated for categorical variables. We considered a two-sided significance level of 0.05 for all tests.
Results: Of 932 SSc patients with a mean age of 59.6 years (20.1-90.5). Of the patients 40% had an interstitial lung disease (ILD) and 12% pulmonary hypertension, respectively. Diffuse cutaneous SSc was present in 226 patients (24%); anti-topoisomerase antibodies were detected in 28%. A DXA scan was available in 38% of the patients. The prevalence of osteoporotic fractures and anti-osteoporotic treatments was 14% and 21%, respectively. Overall, 28% of the cohort was identified as having OPO.
Table 2 compares SSc patients with or without OPO. Besides age and low BMI as strong risk factors, the use of proton-pump inhibitors (OR 1.94, 95%CI 1.38-2.74) and glucocorticoids (OR 3.48, 95%CI 2.57-4.70) were statistically associated with OPO. Cutaneous diffuse form (OR 2.67, 95%CI 1.95-3.76), mRSS above 10 (OR 2.10, 95%CI 1.48-2.96), and anti-topoisomerase antibodies (OR 1.77, 95%CI 1.29-2.41) were associated with OPO. ILD (OR 2.61, 95%CI 1.29-2.41) or symptoms such as NYHA III and IV functional classes (OR 2.13, 95%CI 1.54-2.94), were also positively associated with OPO. The ILD severity, estimated through DLCO alteration and restrictive lung disease, was also associated with OPO. We did not identify any significant association between OPO and calcinosis or vasculopathy, nor oesophageal or gut involvement. CRP and ESR levels were significantly higher in the OPO group (p = 0.004 and p < 0.001, respectively), while haemoglobin levels were significantly lower (p < 0.001).
Conclusion: The prevalence of OPO and fragility fractures in patients with SSc was 28% and 20%, respectively. Beyond classical risk factors, our study suggests that disease severity (as reflected by cutaneous subset, organ involvement, autoantibodies and inflammatory markers) was also associated with bone health in SSc patients.
 Table 1. Patients Characteristics
Table 1. Patients Characteristics
To cite this abstract in AMA style:
Midol C, Wiebe E, Siegert E, Huscher D, Launay D, Hachulla E, Sobanski V, Buttgereit F. Risk of Osteoporosis in Patients with Systemic Sclerosis: A Cross-Sectional Analysis of Two European Prospective Cohorts [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/risk-of-osteoporosis-in-patients-with-systemic-sclerosis-a-cross-sectional-analysis-of-two-european-prospective-cohorts/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/risk-of-osteoporosis-in-patients-with-systemic-sclerosis-a-cross-sectional-analysis-of-two-european-prospective-cohorts/