Session Information
Date: Monday, November 9, 2020
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster III: Bench to Bedside
Session Type: Poster Session D
Session Time: 9:00AM-11:00AM
Background/Purpose: Tubulointerstitial damage in lupus nephritis (LN) is a strong predictor of progression to chronic kidney disease (CKD) and end stage renal disease (ESRD). While prior studies showed complement activation mediates glomerular injury, the role of complement in renal tubular damage has not been evaluated. The objective of this study is to investigate the association between complement activation as measured by tubular complement 9 (C9) deposition with interstitial fibrosis and tubular atrophy (IFTA) in LN.
Methods: LN biopsies from July 2014 to July 2016 were evaluated. Chromogenic immunohistochemistry was performed on formalin-fixed, paraffin-embedded, 4-µm human renal biopsy sections using unconjugated, murine anti-human Complement C9 (Hycult Biotech, clone X197) as a marker of the membrane attack complex (MAC) activation. C3 glomerulopathy was used as a positive control and normal kidney served as a negative control. Tubular basement membrane C9 staining intensity was analyzed as absent (0) versus present (1 to 3) scored on a semi-quantitative scale by a renal pathologist. IFTA was categorized as 0–10%, 11–20%, and >20%. Clinical parameters were assessed at the time of biopsy and 6 months post biopsy.
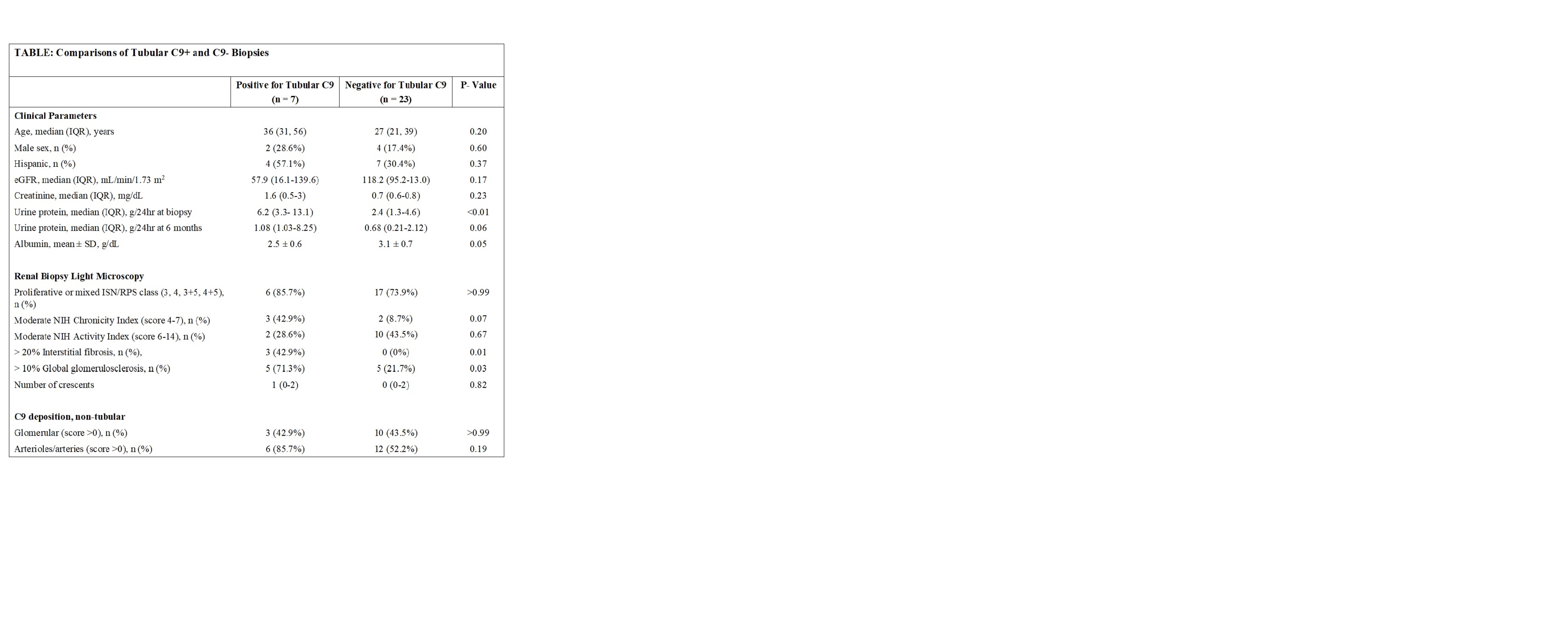
Results: Renal biopsies from 30 LN patients were studied, of which 23 (77%) were proliferative LN. There were 24 (80%) women, mean age 33 (standard deviation) (12) years. Positive tubular C9 staining (C9+) was observed in 7 (23%) biopsies. At the time of renal biopsy, C9+ patients had significantly higher proteinuria, compared to C9- patients: median (interquartile range) 6.2g (3.3-13.1) vs. 2.4g (1.3-4.6), p< 0.01. The differences persisted at 6 months after induction therapy: 1.08g (1.0-8.3) in C9+ vs. 0.68g (0.2-2.1) in C9- patients, p=0.06. Tubular C9 deposition was associated with the finding of interstitial fibrosis on biopsy: 3 out of 7 (42.9%) had >20% interstitial fibrosis as compared to none in the C9- group, p=< 0.01. Higher proportion of C9+ patients had moderate NIH Chronicity index: 3 out of 7 (42.9%) vs 2 out of 23 (8.7%) in the C9- group, p=0.07. There was no significant difference in eGFR at renal biopsy between the two groups.
Conclusion: Tubular C9 deposition is associated with proteinuria, interstitial fibrosis and increased chronicity which are predictors of progression to ESRD. Complement activation may play an important role in tubulointerstitial damage in LN.
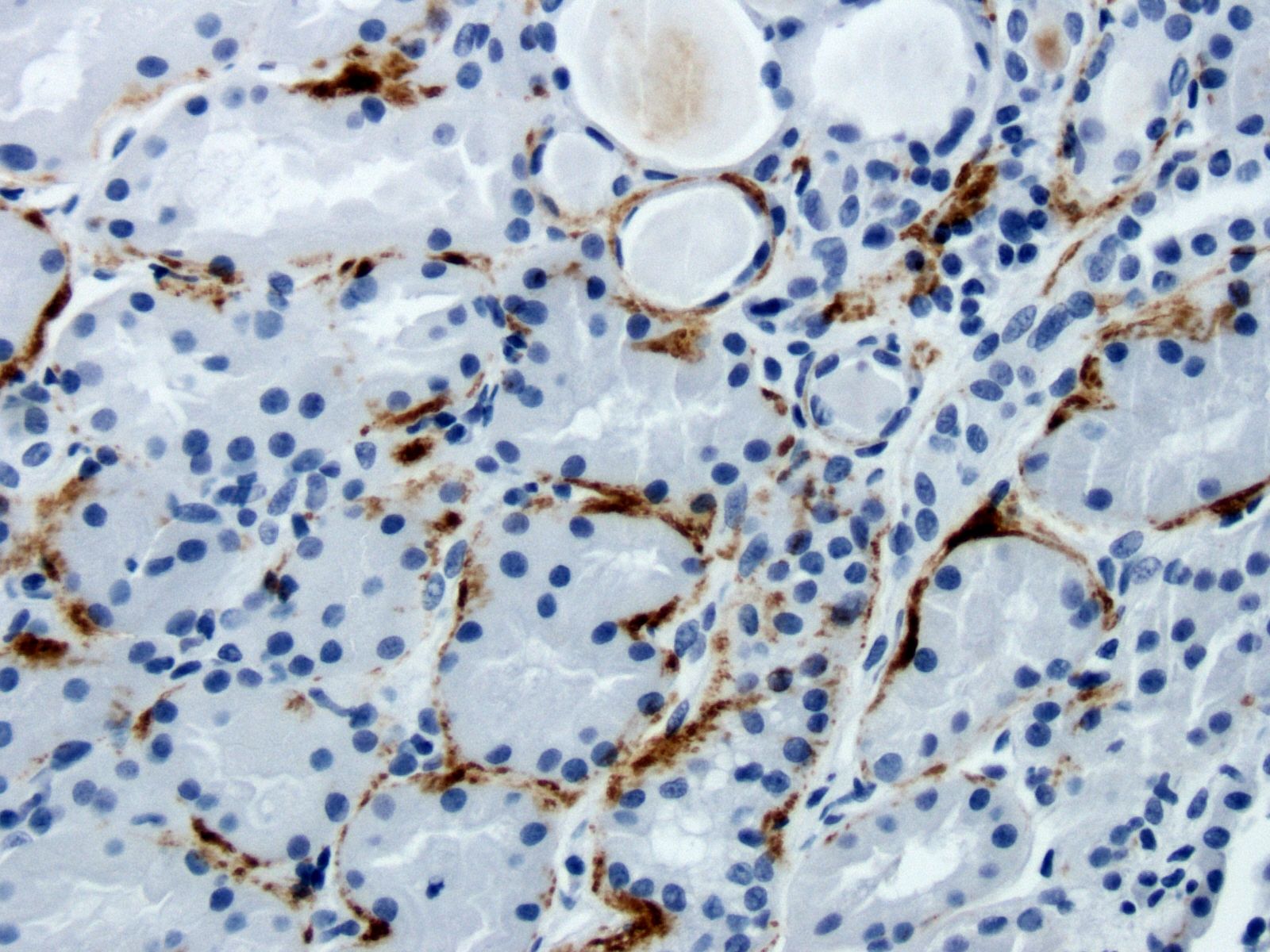 Patient with LN Class V, 2+ tubular C9 deposition and 30 to 40% IFTA.
Patient with LN Class V, 2+ tubular C9 deposition and 30 to 40% IFTA.
To cite this abstract in AMA style:
Wang S, Wu M, Chiriboga L, Goilav B, Wang S, Putterman C, Schwartz D, Pullman J, Broder A, Belmont H. Renal Tubular Complement C9 Deposition Is Associated with Renal Tubular Damage and Fibrosis in Lupus Nephritis [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/renal-tubular-complement-c9-deposition-is-associated-with-renal-tubular-damage-and-fibrosis-in-lupus-nephritis/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/renal-tubular-complement-c9-deposition-is-associated-with-renal-tubular-damage-and-fibrosis-in-lupus-nephritis/