Session Information
Session Type: Abstract Session
Session Time: 3:00PM-3:15PM
Background/Purpose: Social determinants of health (SDOH) operate across individual, family, and community levels. We previously demonstrated that cumulative social disadvantage, comprised of individual and family-level SDOH, was associated with persistent disease activity among children with JIA in the Childhood Arthritis and Rheumatology Research Alliance (CARRA) Registry. However, the role of community-level SDOH, and their interaction with cumulative social disadvantage, in JIA health disparities is unknown.
Methods: In this cohort study of children with JIA in the CARRA Registry (July 2015-January 2022), a cumulative social disadvantage score was generated (range 0-3) for each subject with a score of 1 for each parameter (1) family income < $50,000/year, 2) guardian education at less than high school level, and 3) public or no insurance). Community-level SDOH was assessed using the national Area Deprivation Index (ADI), a measure of neighborhood-level socioeconomic disadvantage geocoded at the census tract level. Descriptive statistics were performed to summarize demographic and clinical characteristics by ADI quartile. Mixed-effects logistic regression models were generated to investigate the association between ADI quartile and active disease (cJADAS-10 >1.1 for oligoarticular JIA; >2.5 for all other subtypes), adjusting for the cumulative social disadvantage score and other covariates. Multiple imputation (50 cycles) addressed missingness in ADI (17%), income (25%), and education (16%). Causal mediation analysis was used to assess the cumulative social disadvantage score and its components as mediators of the association between ADI and disease activity.
Results: Among 9,612 children with JIA, cumulative social disadvantage was more prevalent in the most disadvantaged neighborhoods (Table 1: ADI Q4: 64.9% with score >0 vs. Q1: 18.8%). While ADI was independently associated with persistent disease activity in unadjusted models (ADI Q4: OR 1.43, 95% CI: 1.15-1.76), this was significantly attenuated (ADI Q4: aOR 1.06, 95% CI: 0.85-1.32) upon adjustment for the cumulative social disadvantage score and covariates (Table 2). Cumulative social disadvantage mediated 67.6% of the relationship between most (ADI Q4) versus least (ADI Q1) neighborhood disadvantage and disease activity (Table 3). Low income and insurance mediated 80.2% and 75.2% of this relationship, respectively, while guardian education only mediated 27.0%.
Conclusion: While neighborhood-level deprivation (ADI) was independently associated with persistent disease activity, this relationship was largely mediated by individual and family-level SDOH, particularly household income and insurance status. Therefore, interventions that can address these individual/family-level factors, such as social work and patient navigator services, may be effective strategies for reducing JIA health disparities.
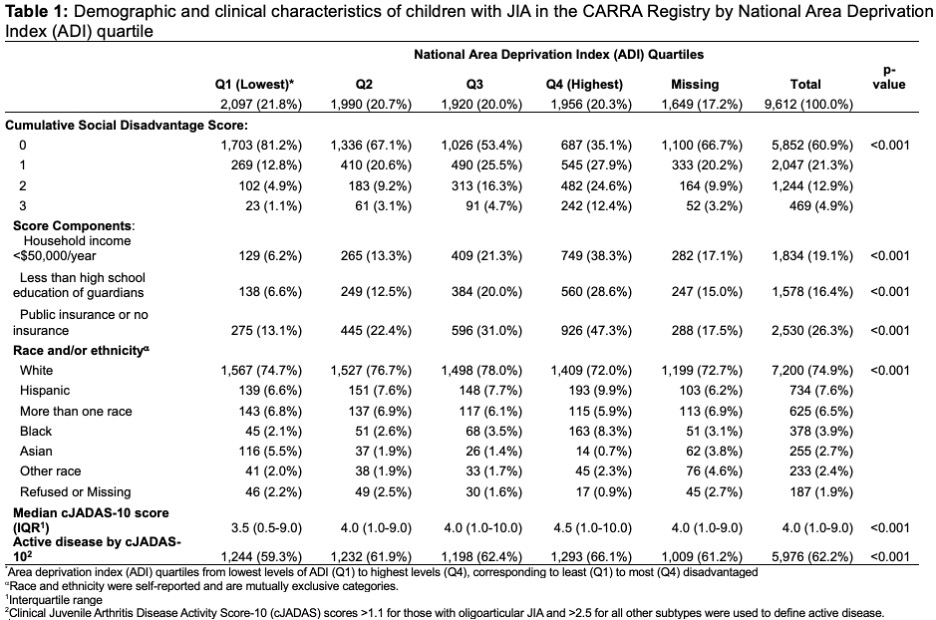 Demographic and clinical characteristics of children with JIA in the CARRA Registry by National Area Deprivation Index (ADI) quartile
Demographic and clinical characteristics of children with JIA in the CARRA Registry by National Area Deprivation Index (ADI) quartile
.jpg) Associations between area deprivation index and cumulative social disadvantage with any active disease throughout Registry follow-up
Associations between area deprivation index and cumulative social disadvantage with any active disease throughout Registry follow-up
.jpg) The adjusted average proportion of the effect of area deprivation index quartile on disease activity mediated by the cumulative social disadvantage score and its components via causal mediation analysis1,2 (n=50 cycles)
The adjusted average proportion of the effect of area deprivation index quartile on disease activity mediated by the cumulative social disadvantage score and its components via causal mediation analysis1,2 (n=50 cycles)
To cite this abstract in AMA style:
Soulsby W, Boscardin J, Horton D, Knight A, Toupin-April K, von Scheven E. Relationships between Neighborhood Disadvantage, Cumulative Social Disadvantage, and JIA Outcomes: A CARRA Registry Study [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/relationships-between-neighborhood-disadvantage-cumulative-social-disadvantage-and-jia-outcomes-a-carra-registry-study/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/relationships-between-neighborhood-disadvantage-cumulative-social-disadvantage-and-jia-outcomes-a-carra-registry-study/
