Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: While OA has been considered a disease of cartilage, early subchondral bone changes may precede cartilage abnormalities. Although higher systemic BMD has a known association with radiographic OA severity, the relation of local subchondral BMD measures at the knee with structural changes on MRI is not well studied. CT topographic mapping of subchondral density is a 3D imaging tool that precisely measures subchondral cortical and trabecular BMD in relation to depth from the subchondral surface, allowing for the study of local knee BMD and its impact on important OA structural outcomes. This study aims to evaluate compartment- and depth-specific subchondral knee BMD in relation to cartilage worsening on knee MRI, with the hypothesis that higher local subchondral knee BMD will be associated with higher risk of cartilage loss in the same compartment.
Methods: Participants from the Multicenter Osteoarthritis (MOST) study, a NIH-funded longitudinal prospective cohort of older adults with or at risk of knee OA, who had knee CTs and MRIs at the 12th year study visit were included in this longitudinal analysis. A 3D imaging tool measuring BMD in relation to depth from the subchondral surface was used to assess proximal tibial subchondral BMD at depths of 0-2.5 mm, 2.5-5.0 mm, and 5-10 mm. Regional analyses of each medial and lateral plateau, at each depth were performed to calculate average BMD. Cartilage worsening on MRI was defined as any increase in the MRI OA Knee Score (MOAKS) subregion score between the 12th year visit and 2-year follow-up, considering the medial and lateral compartment separately. We evaluated the relation of subchondral BMD to compartment-specific cartilage worsening using binomial regression with generalized estimating equations to account for 2 knees within individuals, for each compartment and depth in separate models, and adjusted for age, sex, and body mass index (BMI). We additionally stratified by radiographic OA (ROA) status in separate models.
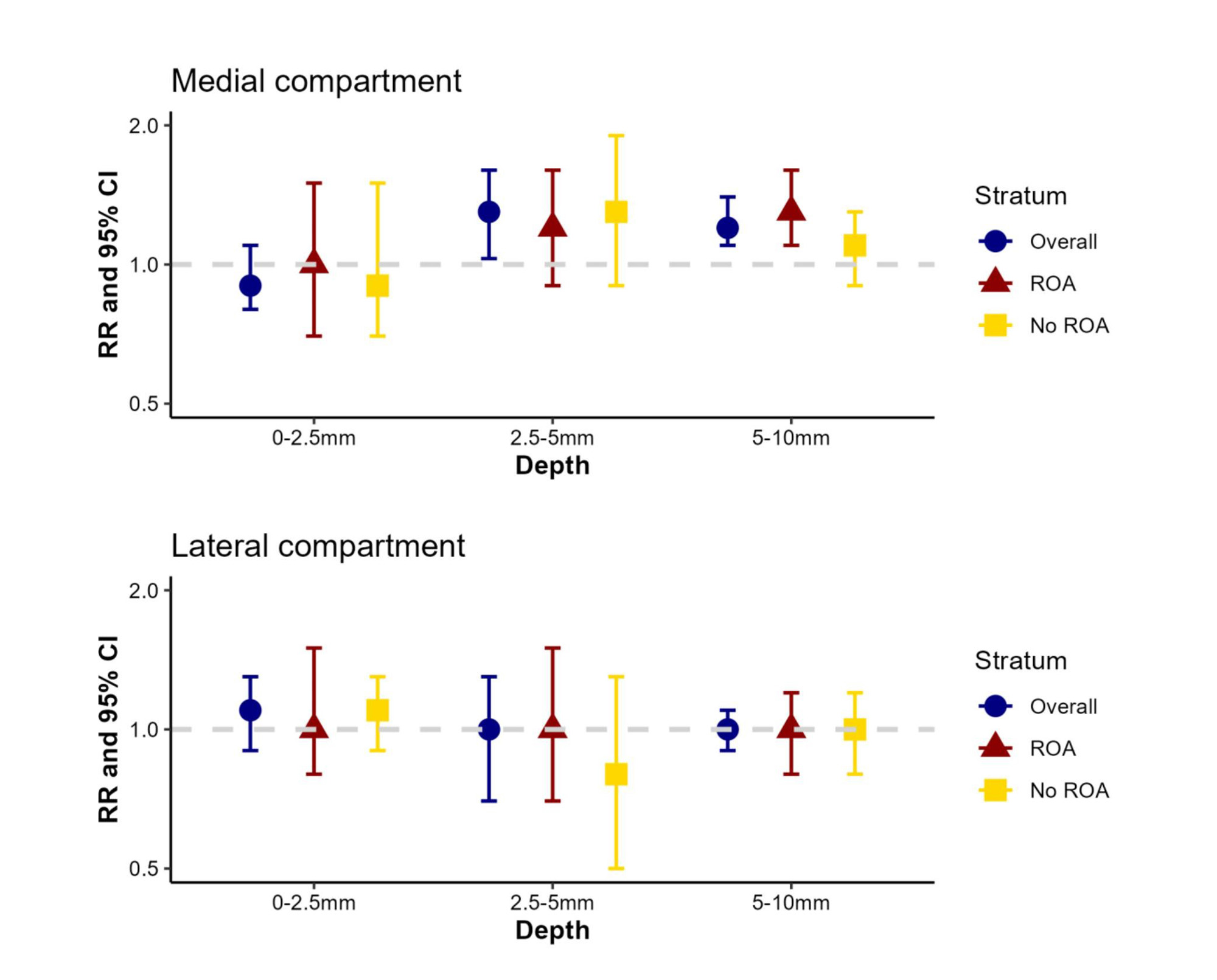
Results: We included 1659 participants (mean age 61 years, 56% female, mean BMI 29 kg/m2). At baseline, 90% of knees had any cartilage damage on knee MRI and 10% had any cartilage worsening at 2-year follow-up. In the medial compartment, at depths of 2.5-10mm below the subchondral surface, the risk of MRI cartilage worsening was 1.2-1.3 times higher for each standard deviation increase in the average subchondral BMD, after confounder adjustment. This association was not seen in the most superficial medial compartment depth (0-2.5mm), nor in the lateral compartment. Analyses stratified by ROA status did not differ substantially from the main results.
Conclusion: Higher subchondral tibial BMD measures were associated with higher risk of cartilage loss in the medial compartment at deeper depths of 2.5-10mm beneath the subchondral surface. These results support differential depth- and compartment-specific contributions from subchondral BMD involved in the pathogenesis of cartilage damage in knee OA.
To cite this abstract in AMA style:
Liew J, Johnston J, Rabasa G, Lewis B, Lynch J, Torner J, Neogi T. Relationship of Depth-Specific Subchondral Bone Mineral Density to MRI Cartilage Worsening: The Multicenter Osteoarthritis Study [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/relationship-of-depth-specific-subchondral-bone-mineral-density-to-mri-cartilage-worsening-the-multicenter-osteoarthritis-study/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/relationship-of-depth-specific-subchondral-bone-mineral-density-to-mri-cartilage-worsening-the-multicenter-osteoarthritis-study/