Session Information
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: OA has traditionally been considered a disease of cartilage but early OA changes in subchondral bone may precede cartilage abnormalities. Altered subchondral bone mineral density (BMD) is thought to lead to cartilage pathology through abnormal force transfer. This in turn may contribute to pain in OA. It is unclear whether BMD increases or decreases with OA, and/or what effect these changes may have on pain. CT topographic mapping of subchondral density (CT-TOMASD) is a 3D imaging tool that precisely measures subchondral cortical and trabecular BMD in relation to depth from the subchondral surface. The aim of this study was to evaluate compartment- and depth-specific subchondral BMD in relation to knee pain.
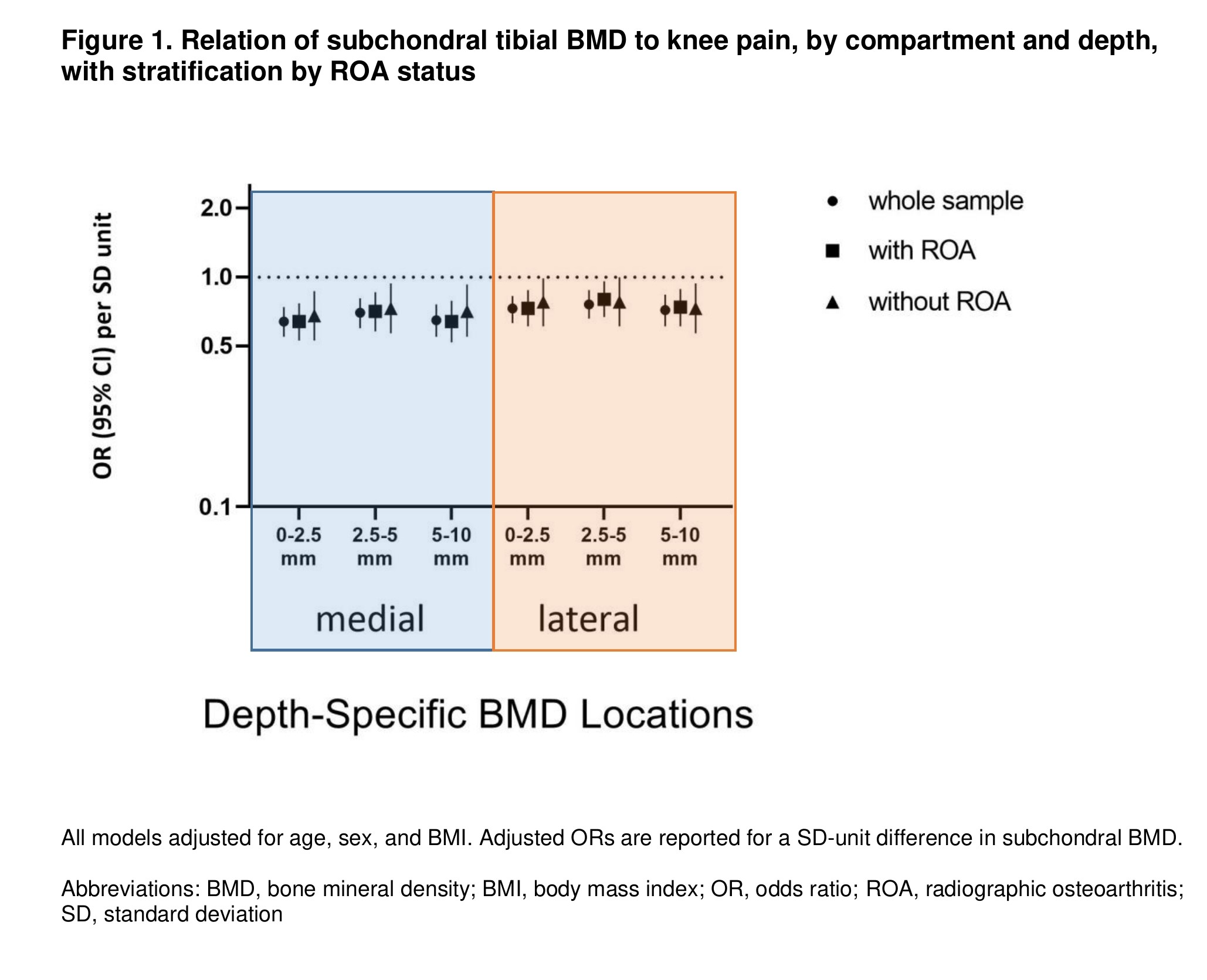
Methods: Participants from the Multicenter Osteoarthritis (MOST) study, a NIH-funded longitudinal prospective cohort of older adults with or at risk of knee OA, who had knee CTs and knee pain assessed were included in this cross-sectional analysis. Knee pain was measured as the mean pain in the past 30 days, scored on a visual analog scale (VAS) (range 0-100), and dichotomized at 40/100. CT-TOMASD was used to assess tibial subchondral BMD at depths of 0-2.5 mm, 2.5-5.0 mm, and 5-10 mm relative to the subchondral surface. Regional analyses of each medial and lateral plateau, at each depth were performed to calculate average BMD. We evaluated the relation of subchondral BMD to presence of knee pain using logistic regression with generalized estimating equations to account for 2 knees within individuals, for each compartment and depth in separate models, and adjusted for age, sex, and body mass index (BMI). We additionally adjusted for, and stratified by, radiographic OA (ROA) status in separate models.
Results: 2082 subjects were included (mean age 61.1±9.7, 56.5% female, mean BMI 28.8±5.2 kg/m2). The odds of having a VAS knee pain of ≥40/100 was significantly lower for a SD-unit increase in average subchondral BMD, after adjustment for age, sex, and BMI. This association was seen in both medial and lateral compartments though more marked within the medial compartment. The magnitude of association did not differ for increasing depths beneath the subchondral surface. Analyses adjusting for, or stratifying by, ROA status did not differ substantially from the main results.
Conclusion: Lower subchondral tibial BMD measures were associated with higher knee pain scores in individuals with or at risk for knee OA. There were no clear differences noted with increasing depths beneath the subchondral surface that would support differential depth-specific contributions from subchondral BMD involved in the pathogenesis of pain in knee OA. These findings may reflect the stage of OA at which there may be high bone remodeling in response to abnormal joint loading, impact or injury, and may be worth exploring as a more timely stage of intervening for targeting OA-related pain. Further studies using CT-TOMASD will evaluate the association of these subchondral BMD measures, including effects of stress-shielding, and structural changes seen on MRI.
To cite this abstract in AMA style:
Liew J, Johnston J, Wang N, Lynch J, Lewis C, Torner J, Neogi T. Relationship of Depth-Specific Subchondral Bone Mineral Density and Pain in Knee Osteoarthritis: The Multicenter Osteoarthritis Study [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/relationship-of-depth-specific-subchondral-bone-mineral-density-and-pain-in-knee-osteoarthritis-the-multicenter-osteoarthritis-study/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/relationship-of-depth-specific-subchondral-bone-mineral-density-and-pain-in-knee-osteoarthritis-the-multicenter-osteoarthritis-study/