Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: There is limited knowledge of the epidemiology and complications of pulmonary manifestations in ANCA-associated vasculitis (AAV). This analysis focused describing the range of pulmonary disease in two forms of AAV: granulomatosis with polyangiitis (GPA) and microscopic polyangiitis (MPA).
Methods: Patients with GPA or MPA enrolled in a prospective longitudinal cohort between April 2006 and December 2023 were included. Patients satisfied a modified ACR 1990 classification criteria for GPA or the Chapel Hill Consensus Conference definition for MPA. Comprehensive data concerning diagnosis, demographics, pulmonary manifestations at onset of disease and/or follow up, and pulmonary damage were collected in a protocolized manner.
Results: Data from 1033 individuals (865 with GPA and 105 with MPA) were included for analysis, including 4511 patient-years of follow up. The mean age at diagnosis was 51.3 years and 55.0% of patients were female. Pulmonary manifestations at any time in the disease course were seen in 70.3% of individuals with AAV: 621 (71.8%) with GPA and 105 (62.5%) with MPA (Figure 1). In GPA, 63.6% had pulmonary involvement at the time of diagnosis and an additional 11.4% at follow-up. In MPA, 56% had manifestations at diagnosis and 4.8% at follow up. Among patients with GPA with pulmonary disease, nodules/cavities were most common manifestation (62.6%); among patients with MPA with pulmonary disease diffuse alveolar hemorrhage was the most common manifestation (61%). Among patients with pulmonary involvement, 285 (45.9%) of those with GPA and 45 (42.9%) of those with MPA had more than one pulmonary manifestation at the same time. 185 (17.9%) individuals had irreversible pulmonary damage, most commonly breathlessness, loss of lung function, or interstitial lung disease (Table 1).
Conclusion: Pulmonary manifestations are common in AAV, differ in frequency between GPA and MPA, and are associated with accumulation of damage. Individuals may have multiple pulmonary manifestations concurrently, suggesting multiple pathophysiologic processes. Systematic assessments of individuals with AAV for pulmonary involvement could potentially lead to earlier detection of these manifestations and reduce pulmonary damage.
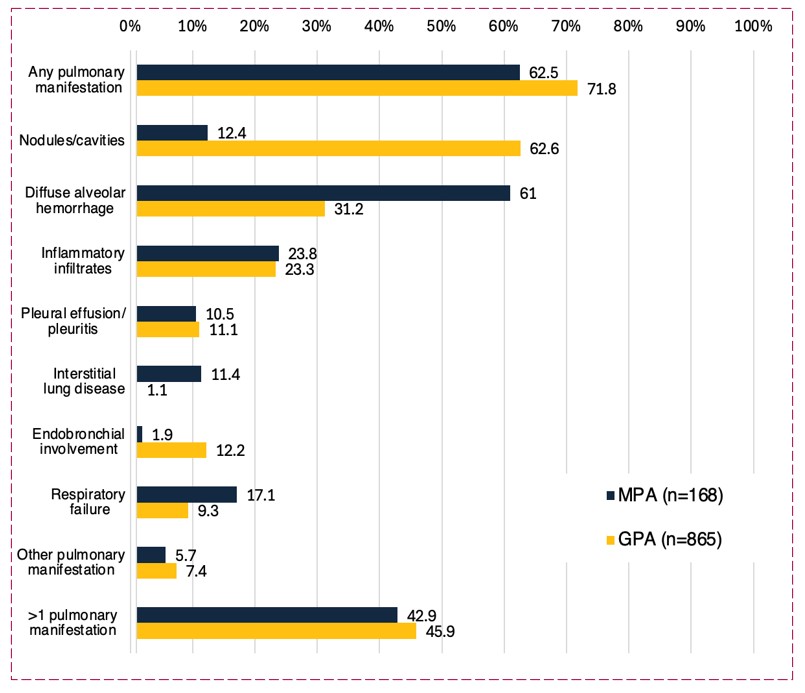 Figure 1: Frequency of pulmonary manifestations in individuals with granulomatosis with polyangiitis (GPA) and microscopic polyangiitis (MPA)
Figure 1: Frequency of pulmonary manifestations in individuals with granulomatosis with polyangiitis (GPA) and microscopic polyangiitis (MPA)
.jpg) Table 1: Pulmonary damage in patients with granulomatosis with polyangiitis
Table 1: Pulmonary damage in patients with granulomatosis with polyangiitis
or microscopic polyangiitis.
To cite this abstract in AMA style:
Junek M, Choi S, Garner S, Rawn S, Cuthbertson D, Koening C, Langford C, McAlear C, Monach P, Moreland L, Pagnoux C, Seo P, Specks U, Warrington K, Cox G, Khalidi N, Merkel P. Pulmonary Manifestations of Granulomatosis with Polyangiitis and Microscopic Polyangiitis [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/pulmonary-manifestations-of-granulomatosis-with-polyangiitis-and-microscopic-polyangiitis/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/pulmonary-manifestations-of-granulomatosis-with-polyangiitis-and-microscopic-polyangiitis/
