Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: RA-associated interstitial lung disease (ILD) is a heterogeneous disease with a chronic course and potential for flares. Serum biomarkers are needed to identify those at risk for RA-ILD progression. The aim of this study was to investigate the associations of baseline and change in pulmonary damage biomarkers (serum Kreb von den Lungen 6 [KL-6], human surfactant protein D [hSP-D], and matrix metalloprotein 7 [MMP7]) with ILD progression among patients with RA-ILD.
Methods: We investigated RA-ILD progression in the Korean RA-ILD (KORAIL) cohort, a prospective, longitudinal observational study that enrolled patients with RA based on 1987 ACR or 2010 ACR/EULAR criteria and ILD on chest computed tomography (CT) scans from January 2015 to July 2018, followed for 3 years. Pulmonary function tests and chest CT scans were conducted annually, and ILD extent on chest CT was scored independently by two radiologists. ILD progression was defined as both physiological and radiological evidence of disease progression adapted from the 2023 ATS/ERS/JRS/ALAT definition of progressive pulmonary fibrosis (PPF). Serum KL-6 level was measured using the latex-enhanced immunoturbidimetric assay method, and hSP-D and MMP7 levels using R-Plex assays. We performed multivariable Cox regression to investigate the associations of biomarkers (baseline value and annual change) with RA-ILD progression, adjusted for age, sex, smoking status, baseline DAS28-ESR score, and baseline biomarker value (in models using annual change in biomarker value).
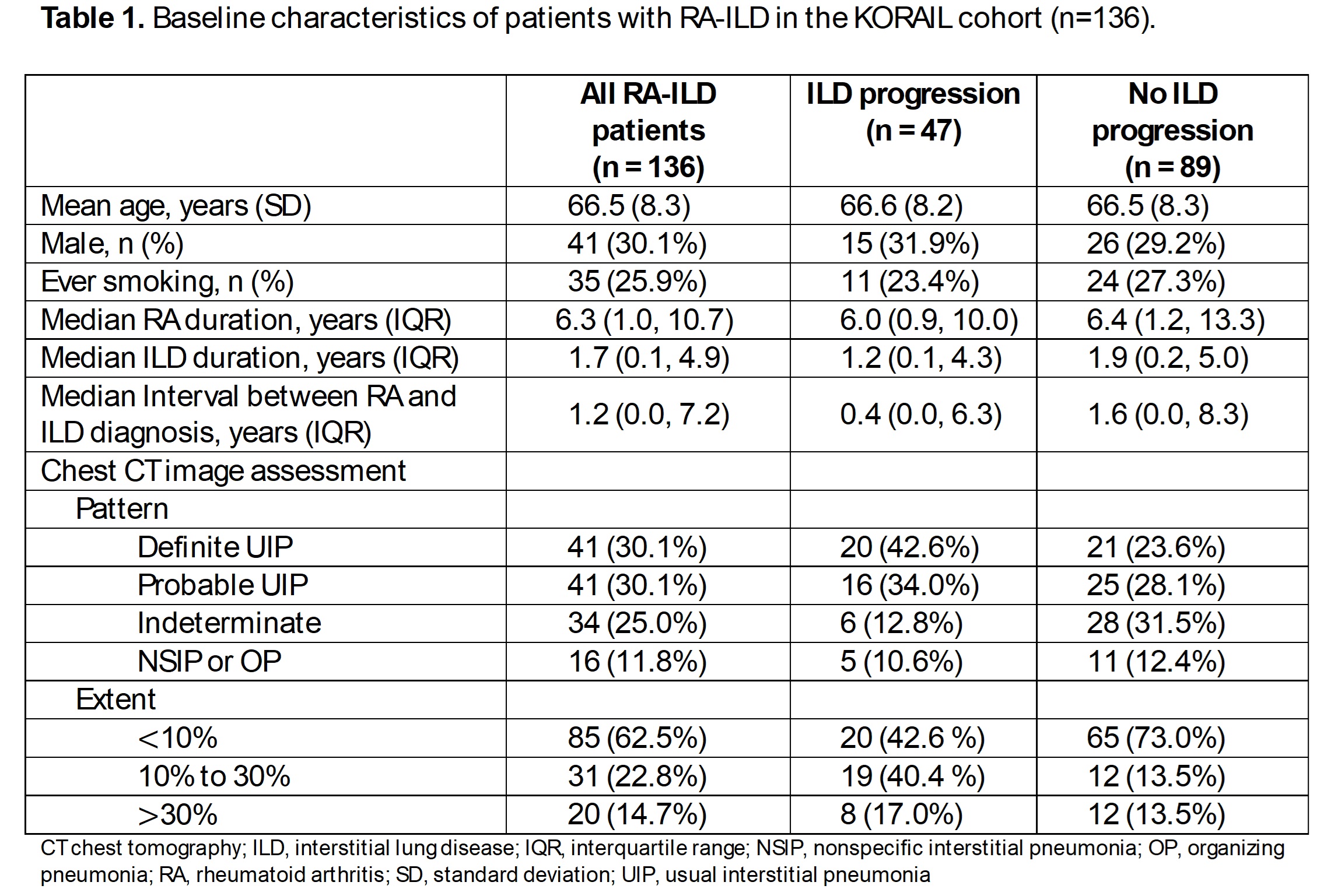
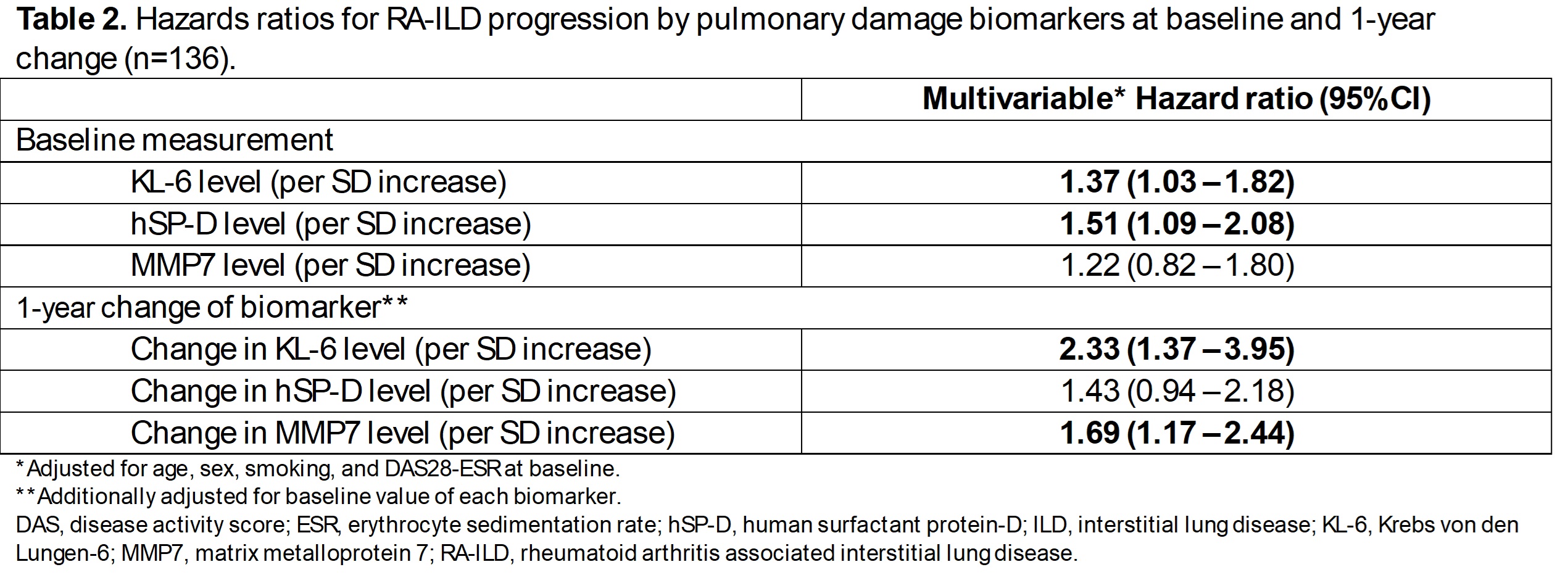
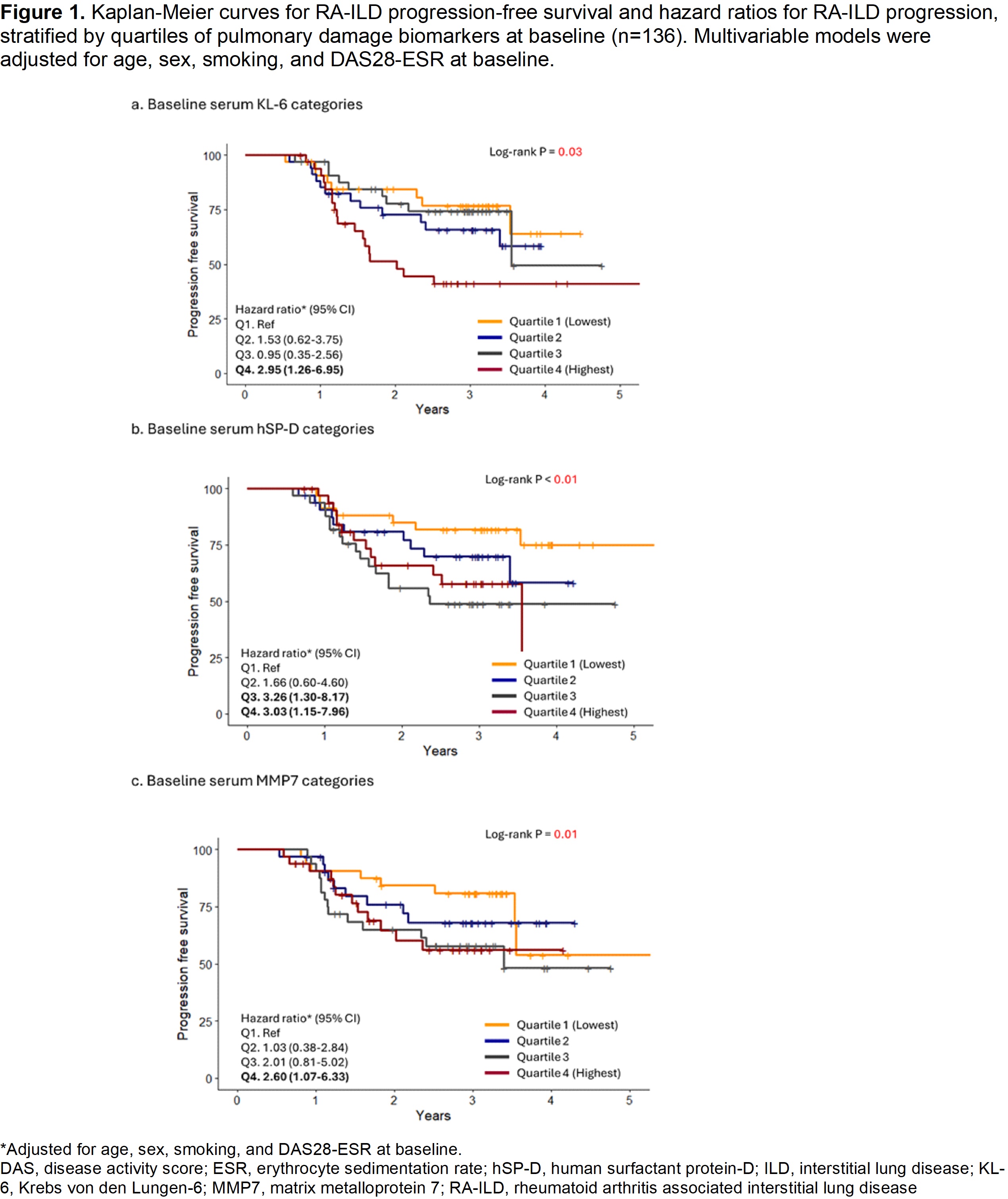
Results: We analyzed 136 RA-ILD patients who had biomarkers measured (mean age 66.5 [SD 8.3] years, 30% male, 60% usual interstitial pneumonia pattern). During a median 3.0 [IQR 2.8, 3.4] years follow-up, 35% (n=47) of patients experienced ILD progression. Higher baseline levels of KL-6 and hSP-D were associated with greater risk of ILD progression (HRs 1.37 per SD increase, 95%CI 1.03-1.82 and 1.51 per SD increase, 95%CI 1.09-2.08, respectively) (Table 1). The highest quartile(Q4) of KL-6 was associated with the worst progression-free survival (HRs 2.95, 95%CI 1.26-6.95 compared to Q1) (Figure 1). Greater annual change in levels of KL-6 and MMP7 were significantly associated with progression in multivariable adjusted models (∆KL-6:HR 2.33 per SD increase in change, 95%CI 1.37-3.95, and ∆MMP7: HR 1.69 per SD increase in change, 95%CI 1.17-2.44). However, annual change in hSP-D was not significantly associated with ILD progression.
Conclusion: In this first longitudinal cohort study to apply recently developed criteria of PPF to RA-ILD, 35% progressed during 3 years of follow-up. Higher baseline levels of KL-6 and hSP-D were associated with RA-ILD progression. In follow-up, greater changes in KL-6 and MMP7 were associated with progression. These data provide evidence that serial measurements of pulmonary damage biomarkers, particularly KL-6, may predict RA-ILD progression and may be helpful in monitoring patients and treatment decisions.
To cite this abstract in AMA style:
Chang S, Park Y, McDermott G, Paudel M, Hayashi K, Ha Y, Lee J, Kim M, Park C, Chung S, Kim J, Ha J, Lee S, Kang E, Lee Y, Choe J, Lee E, Sparks J. Pulmonary Damage Biomarkers and Progression of Rheumatoid Arthritis-associated Interstitial Lung Disease in a Prospective Longitudinal Cohort [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/pulmonary-damage-biomarkers-and-progression-of-rheumatoid-arthritis-associated-interstitial-lung-disease-in-a-prospective-longitudinal-cohort/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/pulmonary-damage-biomarkers-and-progression-of-rheumatoid-arthritis-associated-interstitial-lung-disease-in-a-prospective-longitudinal-cohort/