Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Autoantibodies, e.g., against citrullinated proteins (ACPA), increase the risk of clinical arthritis and can be detected years before rheumatoid arthritis (RA) onset. EULAR’s definition of clinically suspect arthralgia (CSA) helps to differentiate patients at risk of RA from those with other types of arthralgia. We previously identified a shift towards pro-inflammatory monocyte subsets in individuals at risk for RA. CD11c, involved in pro-inflammatory cytokine production, is highly expressed in the mononuclear cells of RA patients. We aimed to study monocyte subsets and CD11c expression in at-risk individuals with arthralgia.
Methods: Individuals from the At Risk of RA (ARRA) prospective observational cohort were defined as having arthralgia without clinical arthritis at baseline and being either ACPA+ and/or meeting the EULAR definition of CSA (further CSA+).
Baseline peripheral blood samples were analyzed using flow cytometry. Monocytes were classified into classical (CD14++CD16-), intermediate (CD14++CD16+/++), and nonclassical (CD14-/+CD16++) subsets. CD11c membrane expression was assessed in each subset. Ultrasound (US) synovitis was evaluated using GLOESS and US7 scores. Data were analyzed using the Mann-Whitney test and Spearman’s correlation, expressed as a median and interquartile range [IQR].
Results: Out of 207 at-risk individuals (median symptom duration of 14 months), 46 developed clinical arthritis (progressors) within a median of 8 months of follow-up and 30.45 [14.55-67.88] months of symptom duration, with CRP 5.50 [2.09-14.10] mg/l and DAS28-CRP score 4.46 [3.10-5.23] at arthritis onset. Individuals who had not yet progressed to arthritis with symptom duration >12 months at the latest assessment were defined as non-progressors (n=151).
In the entire cohort, there were no significant differences in the % of monocyte subsets between ACPA+/ACPA- or CSA+/CSA- individuals. However, ACPA+ individuals had higher CD11c expression in both classical (p=0.024) and nonclassical (p=0.040) monocyte subsets than ACPA- individuals. No differences in monocyte subsets were observed between progressors and non-progressors, but ACPA+ progressors meeting CSA criteria had higher CD11c expression in classical (p=0.030) and nonclassical (p=0.015) monocytes and a trend towards higher expression in intermediate (p=0.062) monocytes when compared to all non-progressors.
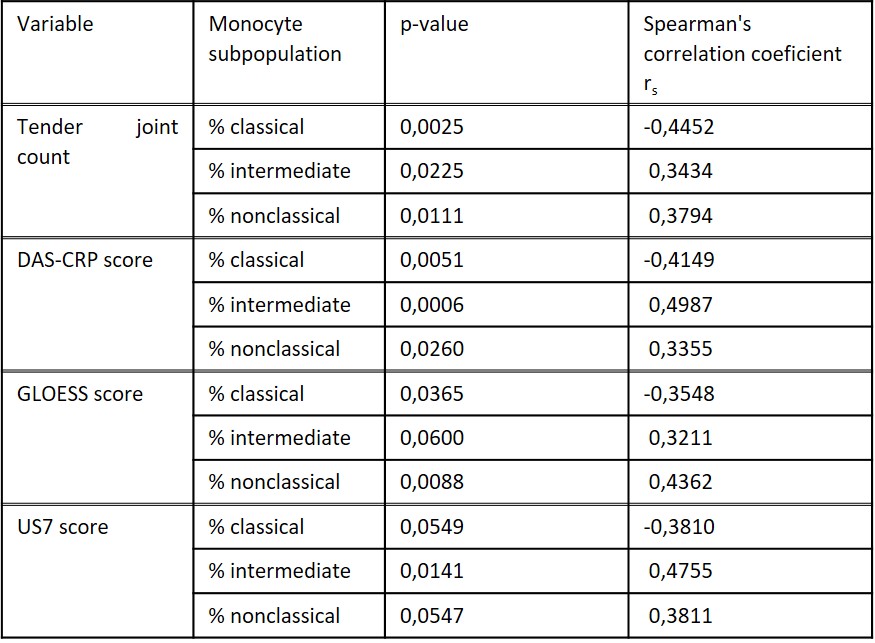
In progressors; baseline % of intermediate and nonclassical monocytes positively correlated with baseline tender joint count, DAS-CRP, and US-detected subclinical synovitis (GLOESS and US7 score), while classical monocytes correlated with these parameters negatively (Table 1). No such correlations were seen at arthritis onset or in non-progressors.
Conclusion: We show increased CD11c expression in monocytes of ACPA+ individuals at risk for RA, particularly in progressors meeting CSA criteria. The positive correlation of pro-inflammatory monocyte subsets with subclinical activity, assessed before the development of clinical arthritis, suggests their potential role in RA pathogenesis.
Acknowledgement: Projects NU22-05-00226, MHCR-023728, SVV-260638
To cite this abstract in AMA style:
Prajzlerová K, Kryštufková O, Hánová P, Růžičková N, Hulejová H, Vencovský J, Šenolt L, Filková M. Pro-inflammatory Monocytes and CD11c Expression in ACPA Positive Individuals with Arthralgia and Their Associations with Subclinical Synovitis Preceding the Onset of Arthritis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/pro-inflammatory-monocytes-and-cd11c-expression-in-acpa-positive-individuals-with-arthralgia-and-their-associations-with-subclinical-synovitis-preceding-the-onset-of-arthritis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/pro-inflammatory-monocytes-and-cd11c-expression-in-acpa-positive-individuals-with-arthralgia-and-their-associations-with-subclinical-synovitis-preceding-the-onset-of-arthritis/