Session Information
Date: Wednesday, November 15, 2023
Title: Abstracts: Miscellaneous Rheumatic & Inflammatory Diseases III
Session Type: Abstract Session
Session Time: 9:00AM-10:30AM
Background/Purpose: Interstitial pneumonia with autoimmune features (IPAF) is a subset of interstitial lung disease (ILD) that manifests with interstitial pneumonia and features of autoimmunity while not meeting classification criteria for a defined rheumatic disease. Recent studies have examined the clinical characteristics, common comorbidities, and outcomes of IPAF patients, but little is known regarding the presence of pulmonary hypertension (PH) in this population. Given the known effect of PH on decreased functional capacity and increased mortality in patients with underlying ILD, we characterize the effect of PH on lung disease progression and mortality in a cohort of patients with IPAF.
Methods: Using a retrospective study design, we evaluated the prevalence of PH in an institutional cohort of patients with IPAF at the University of Texas Southwestern Medical Center. Included patients were identified as having pre-capillary PH on right heart catheterization as defined by the European Society of Cardiology 2022 guidelines. Descriptive statistics were used to describe baseline data including demographic factors, radiographic patterns, pulmonary function tests, and 6-minute walk distance. In addition, right heart catheterization (RHC) and echocardiogram (TTE) data were collected and used to stratify patients according to disease severity (severe = mean pulmonary artery pressure (mPAP) ≥30 mmHg and pulmonary vascular resistance (PVR) ≥4 WU). Using Cox logistic regression, we evaluated the association of clinical variables on time to relative forced vital capacity (FVC) decline of ≥10% and survival.
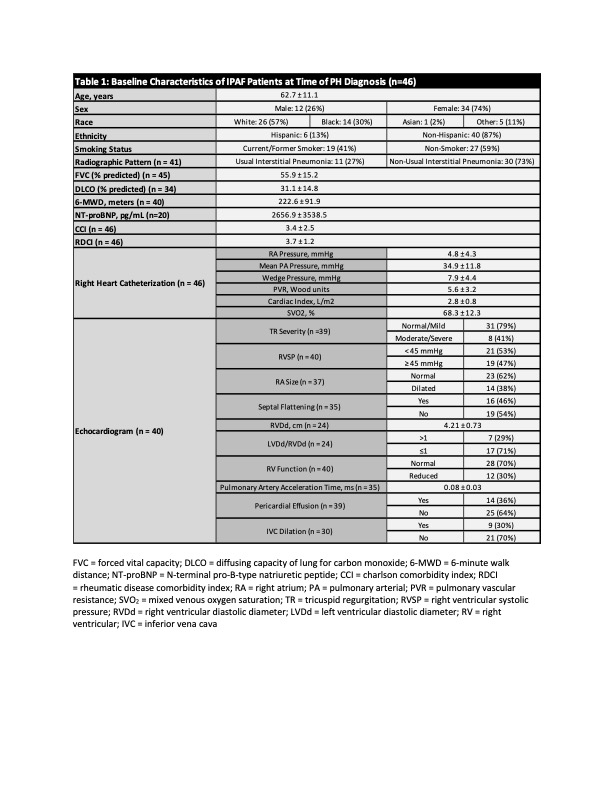
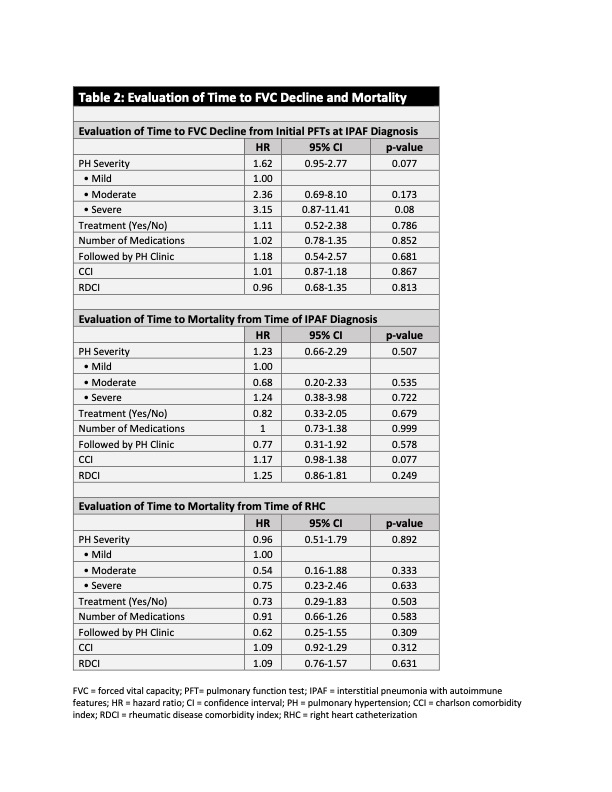
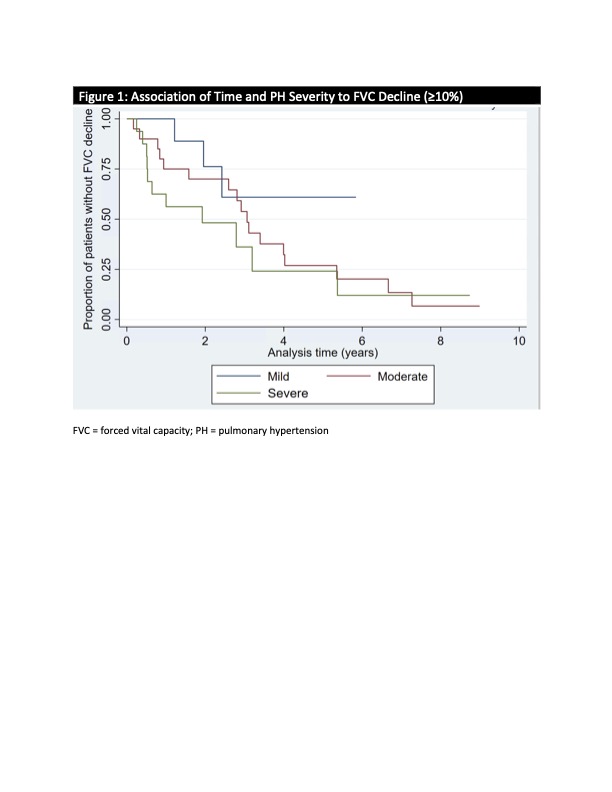
Results: A cohort of 173 IPAF patients was analyzed, of which 46 patients (26.6%) met criteria for pre-capillary PH by RHC. Clinical characteristics of the patients with PH are summarized in Table 1. Among the patients with PH by RHC (n=46), 21 (46%) were classified as having mild or moderate PH, and 25 (54%) with severe PH. The average time between IPAF and PH diagnosis was 2.35 (SD ± 2.1) years. Following diagnosis, 92% of patients with severe PH were followed in PH clinic and started on treatment. There was not a statistically significant association between the severity of PH, being followed in PH clinic, or the number of PH medications and time to relative FVC decline ≥10% or mortality (Table 2). A trend was observed as patients with more severe PH had a faster decline in FVC of 10% or more (Figure 1).
Conclusion: PH was prevalent in our cohort of patients with IPAF and the severity of PH was associated with lung function decline and mortality, although this was not statistically significant. Clinicians taking care of patients with IPAF should be aware of the high prevalence of PH and its possible association with clinical outcomes in this population. Thus, a high index of suspicion for the condition should be maintained when a patient with IPAF is evaluated, and further screening and workup should be considered if PH is suspected.
To cite this abstract in AMA style:
Ghebranious M, Joerns E, Adams T, Shah T. Prevalence of Pulmonary Hypertension in a Cohort of Patients with Interstitial Pneumonia with Autoimmune Features and Its Effect on Lung Disease Progression and Mortality [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/prevalence-of-pulmonary-hypertension-in-a-cohort-of-patients-with-interstitial-pneumonia-with-autoimmune-features-and-its-effect-on-lung-disease-progression-and-mortality/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prevalence-of-pulmonary-hypertension-in-a-cohort-of-patients-with-interstitial-pneumonia-with-autoimmune-features-and-its-effect-on-lung-disease-progression-and-mortality/