Session Information
Date: Sunday, November 7, 2021
Session Type: Poster Session B
Session Time: 8:30AM-10:30AM
Background/Purpose: Non-treatment and treatment delays contribute to suboptimal symptom control and irreversible joint damage in patients with inflammatory arthritis (IA). This investigations objective was to identify baseline patient factors associated with treatment initiation during the 12 months after the initial diagnosis of rheumatoid arthritis (RA), psoriatic arthritis (PsA), or ankylosing spondylitis (AS).
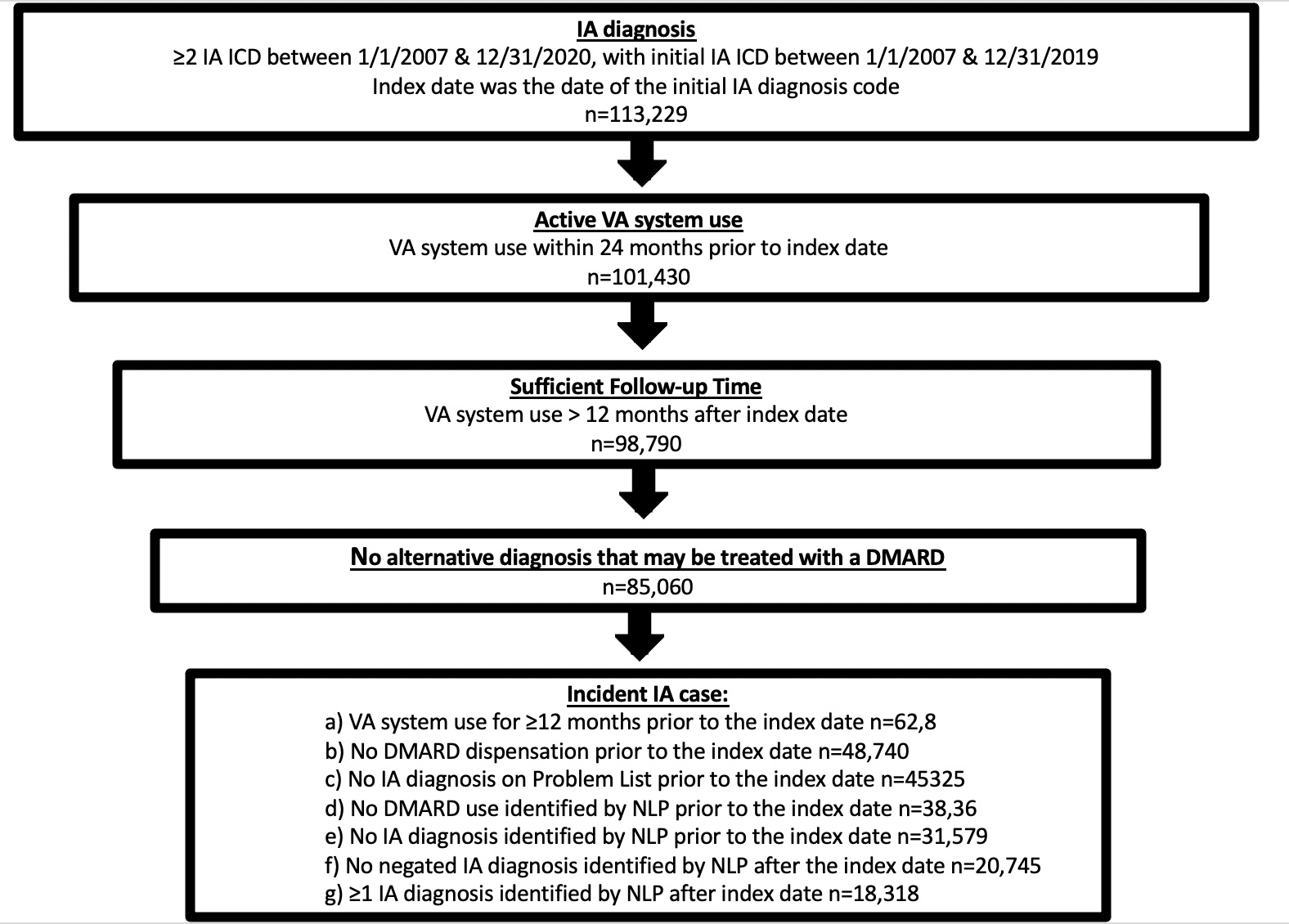
Methods: Active users of the Veteran Affairs Health System with an incident IA diagnosis between 1/1/2007 and 12/31/2019 were included (Figure 1). Data resources included the corporate data warehouse and the VA Informatics and Computing Infrastructure. Coded data were used to identify comorbidities, medications, laboratory data, provider visits and other encounters in the VA system. Natural language processing improved the accuracy of incident cohort identification and identifying erosions due to IA in the text of radiology reports. Treatment was captured during the 12 months following the initial IA diagnosis. Univariate analysis was used to explore patient factors associated with treatment. In normally distributed continuous variables means and standard deviations were compared, while medians and interquartile ranges were used for non-normally distributed variables.
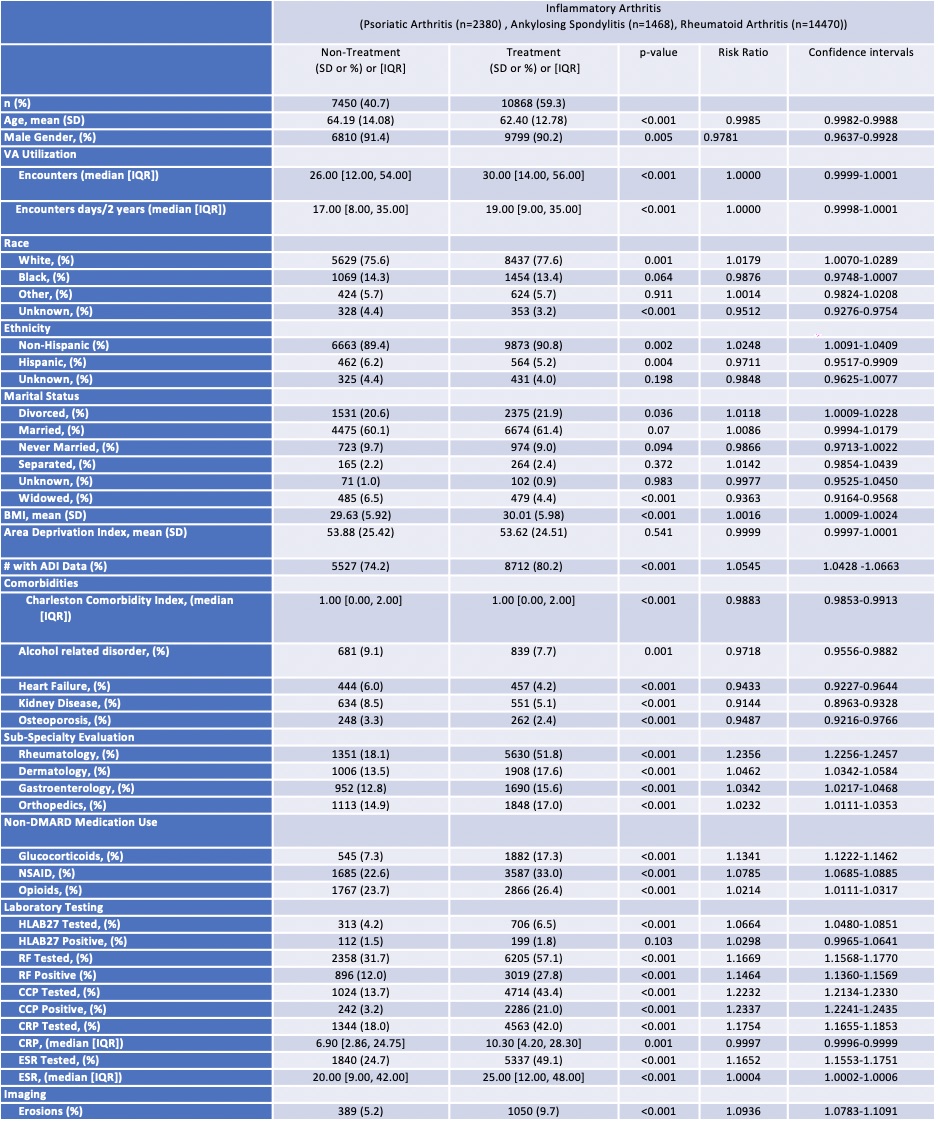
Results: The study included 18,318 Veterans with incident IA (14,470 RA, 2380 PsA, 1468 AS). The mean age was 63.1 years and 90.7% were male. In the 12 month follow-up period, 40.7% did not use an IMM. VA system utilization was similar between groups (RR=1.000). Characteristics significantly associated with treatment included younger age (RR=0.9985), female gender (RR=0.9781), white race (RR=1.0179) non-Hispanic ethnicity (RR=1.0248), divorced marital status (RR=1.0118), and higher BMI (RR=1.0016). Estimates of socioeconomic status (measured by the area deprivation index [ADI]) were similar amongst patients with available data, but treatment was less frequent in patients with missing ADI (RR=1.0545). Higher comorbidity burden (RR=0.9883), alcohol dependence (RR=0.9718), heart failure (RR=0.9433), kidney disease (RR=0.9144), and osteoporosis (RR=0.9487) associated with non-treatment. Rheumatology (RR=1.2356), dermatology (RR=1.0462), gastroenterology (RR=1.0342), and orthopedic (RR=1.0232) visits were associated with treatment. Use of glucocorticoids (RR=1.1341), NSAIDS (RR=1.0785), and opiates (RR=1.0214) associated with treatment. Tests associated with therapy included: HLA-B27, RF, CCP, CRP, ESR. Positive results with RF, CCP, ESR, and articular erosions were associated with treatment (Table 2).
Conclusion: Several patient factors including certain demographics, subspecialty visits, additional medications, laboratory testing and erosions on imaging had a positive association with treatment. Other patient factors such as male gender, comorbidities and unknown addresses had a negative association with treatment. Future research with added analyses of these factors (multivariate analysis) and additional factors (health system and provider variables) may inform strategies to improve early treatment in appropriate patients with IA.
To cite this abstract in AMA style:
Braaten T, Pei s, Rathod A, Penmetsa G, Douglas K, Walker J, Clewell J, Walsh J. Predictors of Treatment for Inflammatory Arthritis with Immune Modulating Medications (IMM) in US Veterans [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/predictors-of-treatment-for-inflammatory-arthritis-with-immune-modulating-medications-imm-in-us-veterans/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/predictors-of-treatment-for-inflammatory-arthritis-with-immune-modulating-medications-imm-in-us-veterans/