Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Evidence suggests that patients with autoimmune diseases or immunosuppressive conditions have a higher risk of poor outcomes related to Coronavirus disease 2019 (COVID-19) infection. Additionally, they are more likely to have persistent symptoms after the resolution of the acute illness, which is known as Post-Acute Sequelae of SARS-CoV-2 infection (PASC), or Long COVID. In studies that have examined the associations between COVID-19, PASC, and rheumatic diseases, Rheumatoid Arthritis (RA) represents a significant fraction of this patient population. We aim to compare patients with RA who have developed PASC to other patients with RA who have not developed PASC to determine risk factors that could predict the occurrence of this condition.
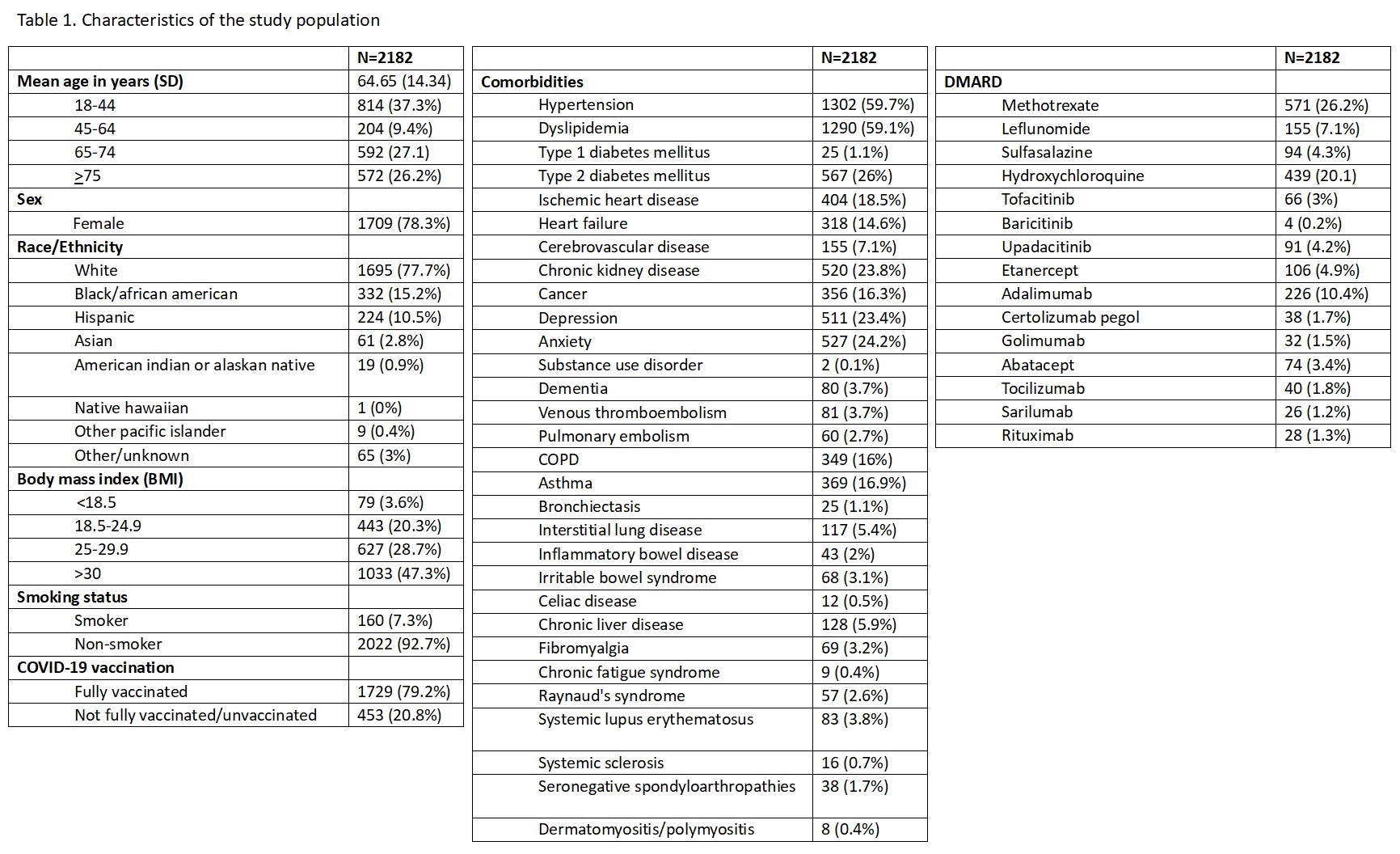
Methods: This was a retrospective case-control study with patients from the Advocate Aurora health system, between October 2021 and August 2023. We included patients 18 years and older with RA and a history of a previous COVID-19 infection. Subsequently, they were divided into two groups based on whether they had an existing diagnosis of PASC (cases) or not (controls). Patients diagnosed with Fibromyalgia or Chronic Fatigue Syndrome at any time after a COVID-19 infection were excluded. Our variables of interest included demographic features, body mass index (BMI), smoking status, COVID-19 vaccination status, comorbidities, and disease-modifying antirheumatic drug (DMARD) regimen. All the data was collected using Epic Electronic Health Record’s Slicer Dicer tool. Multivariable logistic regression was conducted to explore the association between PASC and relevant risk factors.
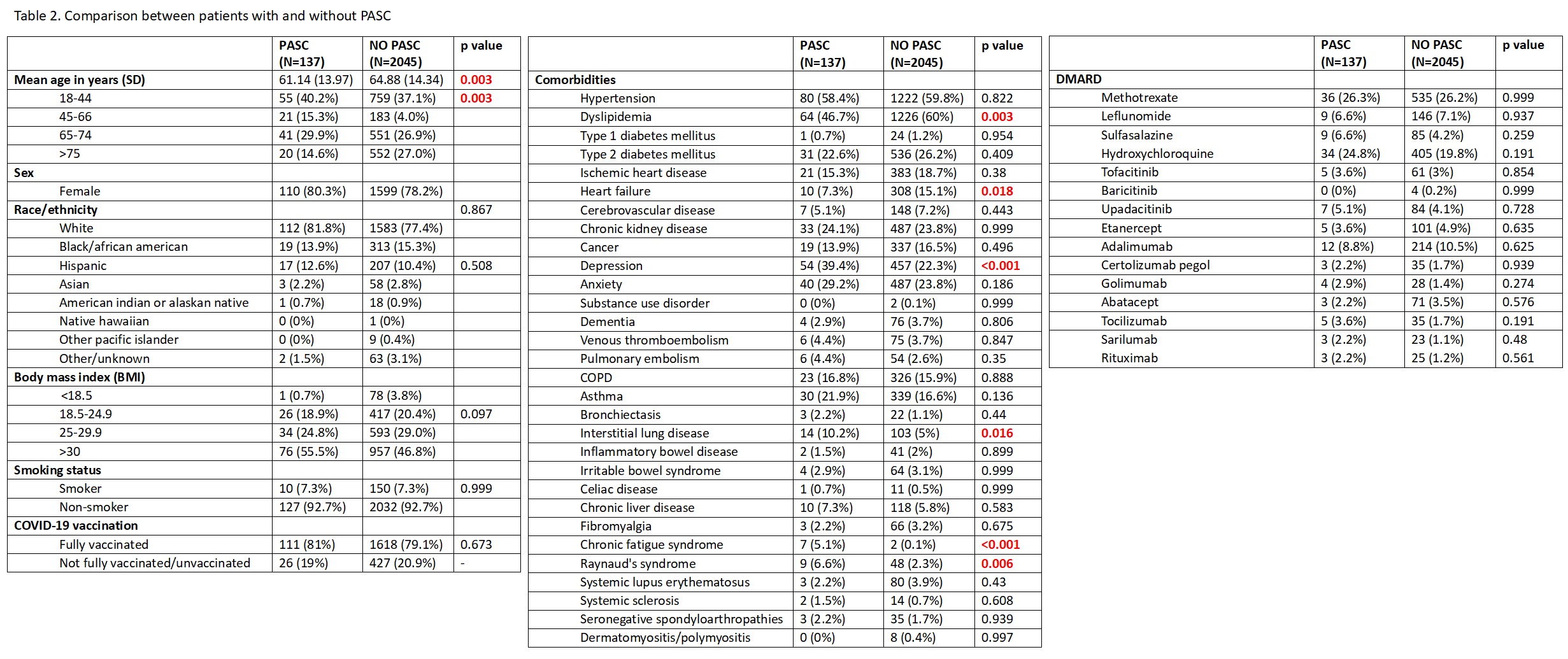
Results: From a total of 2182 RA patients, we identified 137 (6.27%) with a diagnosis of PASC. Patients with PASC were found to be younger than those without PASC (mean age in years 61.14 [SD=13.97] vs. 64.88 [SD=14.34]), with the most statistical significance observed in the age group of 18-44 years (p=0.003). In patients without PASC, there was a higher prevalence of Dyslipidemia (1226 [60%] vs. 64 [46.7%], p=0.003) and Heart Failure (308 [15.1%] vs. 10 [7.3%], p=0.018). In patients with PASC, there was a higher prevalence of Depression (54 [39.4%] vs. 457 [22.3%], p< 0.001), Interstitial Lung Disease (14 [10.2%] vs. 103 [5%], p 0.016), Chronic Fatigue Syndrome (7 [5.1%] vs. 2 [0.1%], p< 0.001), and Raynaud’s syndrome (9 [6.6%] vs. 48 [2.3%], p=0.006). No statistically significant differences were observed when comparing other demographic, clinical, or pharmacological data.
Conclusion: We identified statistically significant risk factors associated with PASC, which included younger age, Depression, Interstitial Lung Disease, Chronic Fatigue Syndrome, and Raynaud’s syndrome. We encourage further studies to validate these findings. In addition, future investigations should aim for higher statistical power to determine the true effect of DMARD in this patient population. Epic Electronic Health Record’s Slicer Dicer tool greatly facilitated data extraction; thus, we believe it should be more widely used in this type of research, especially in large health systems.
To cite this abstract in AMA style:
Lopez Castillo E, Ording J. Predictors of Post-acute Sequelae of COVID-19 in Patients with Rheumatoid Arthritis: A Retrospective Analysis of a Large Health System in the Midwestern United States [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/predictors-of-post-acute-sequelae-of-covid-19-in-patients-with-rheumatoid-arthritis-a-retrospective-analysis-of-a-large-health-system-in-the-midwestern-united-states/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/predictors-of-post-acute-sequelae-of-covid-19-in-patients-with-rheumatoid-arthritis-a-retrospective-analysis-of-a-large-health-system-in-the-midwestern-united-states/