Session Information
Session Type: Abstract Session
Session Time: 1:00PM-2:30PM
Background/Purpose: Quantifying healthcare inequality is essential to addressing the imbalance in outcomes attributable to age, gender, ethnicity and multimorbidity. In this study, we analysed differences in the initiation of biologic or targeted synthetic DMARDs (b/tsDMARDs) in patients with RA within the universal healthcare system of England and Wales
Methods: An observational cohort study was conducted using the National Early Inflammatory Arthritis Audit (NEIAA) dataset, which enrols patients newly referred with inflammatory arthritis diagnoses in England and Wales. We included all patients with RA who were enrolled in NEIAA between May 8, 2018, and April 30, 2022, and who had 12-month follow-up data available. Modified Poisson regression was used to explore factors associated with the initiation of b/tsDMARDs within 12 months of initial rheumatology assessment.
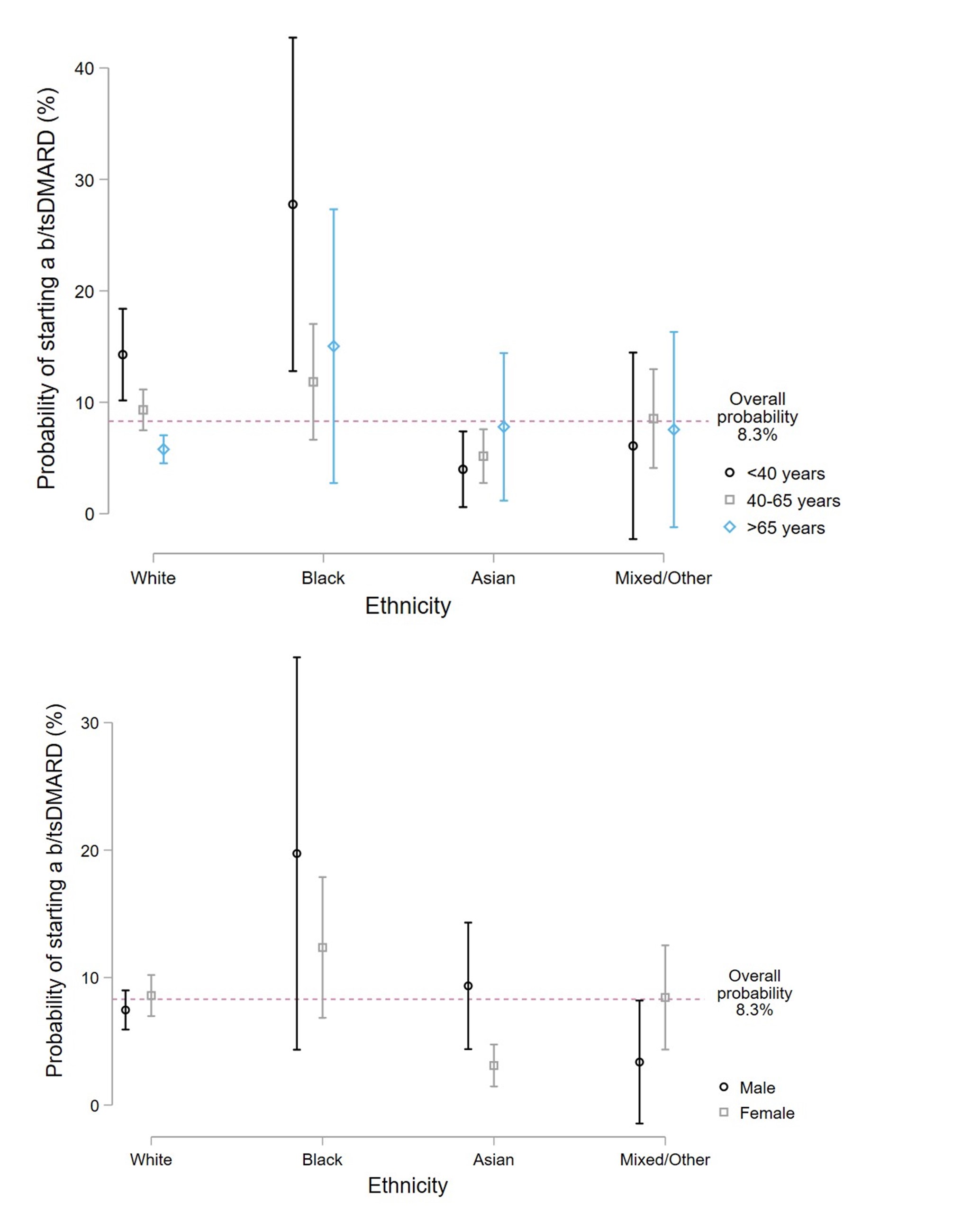
Results: Of 6,098 RA patients with available follow-up, the mean age was 59.2 years (SD 14.9); 3,912 (64.2%) patients were female; 6,047 (99.2%) patients had available ethnicity data, of whom 5,215 (86.2%) were White, 152 (2.5%) were Black, 478 (7.9%) were Asian, and 202 (3.3%) were of mixed or other ethnicities. 508/6,098 (8.3%) patients initiated b/tsDMARDs within 12 months of their initial rheumatology assessment. Patients aged < 40 years were more likely to be initiated on b/tsDMARDs than individuals > 65 years (multivariable-adjusted risk ratio [aRR] 2.41; 95% CI 1.83 to 3.19; p < 0.0001). Individuals of Asian ethnicity were nearly 50% less likely to be initiated on b/tsDMARDs than White individuals (aRR 0.52; 95% CI 0.36 to 0.76; p=0.0007), which persisted after adjustment for socioeconomic status, comorbidities, baseline disease severity, and the initial response to conventional synthetic DMARDs (Figure 1). These differences were evident for Asian females but not Asian males. Individuals of Black ethnicity were more likely to be initiated on b/tsDMARDs than White individuals (aRR 1.54; 95% CI 1.10 to 2.16; p=0.012), which became non-significant after adjusting for baseline disease severity and seropositivity status.
Conclusion: The initiation of b/tsDMARDs for patients with newly diagnosed RA varies markedly by ethnicity and age, despite England and Wales having a universal healthcare system. Our study demonstrates the importance of providing tailored information and ensuring equitable access to high-quality care for underserved patient groups. The one-size-fits-all approach must be reconsidered if health disparities are to be mitigated effectively.
To cite this abstract in AMA style:
Russell M, Gibson M, Zuckerman B, Kumar K, Dubey S, Adas M, Alveyn E, Patel S, Yang Z, Bechman K, Price E, Gallagher S, Cope A, Norton S, Galloway J. Predictors of Biologic and Targeted Synthetic DMARD Initiation for Rheumatoid Arthritis Across Underserved Patient Groups: Insights from a National Cohort Study [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/predictors-of-biologic-and-targeted-synthetic-dmard-initiation-for-rheumatoid-arthritis-across-underserved-patient-groups-insights-from-a-national-cohort-study/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/predictors-of-biologic-and-targeted-synthetic-dmard-initiation-for-rheumatoid-arthritis-across-underserved-patient-groups-insights-from-a-national-cohort-study/