Session Information
Date: Sunday, October 26, 2025
Title: (0280–0305) Muscle Biology, Myositis & Myopathies – Basic & Clinical Science Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Dermatomyositis (DM) is a chronic systemic autoimmune disease with a heterogenous clinical course. Flares often lead to increased morbidity, health care utilization, and reduced quality of life. Understanding risk factors and clinical features of flares can inform individualized therapeutic and monitoring strategies. In this study, we aim to determine the predictors and characteristics of flares in patients with DM.
Methods: Patients who were seen at the Myositis Center outpatient clinic and fulfilled the 2017 EULAR/ACR Classification Criteria for DM were included. Two authors manually reviewed all notes to ascertain any increase in disease activity and the context in which it occurred. Patient symptoms, physical exams, labs, imaging findings, and medication changes were recorded for each encounter. Objective flare was defined as evidence of active disease on exam or ancillary testing (worsening/new weakness, rash, inflammatory arthritis, pulmonary function test [PFT] or lung imaging findings concerning for worsening/new myositis-related lung disease) that resulted in an increase in immunosuppressive therapy. Increased disease activity within 6 months of diagnosis were not counted, nor were increases in disease activity within 3-6 months after tapering immunosuppression. The characteristics of participants and flares were summarized using descriptive statistics. We assessed the association between covariates and time to first flare using Cox proportional hazards models.
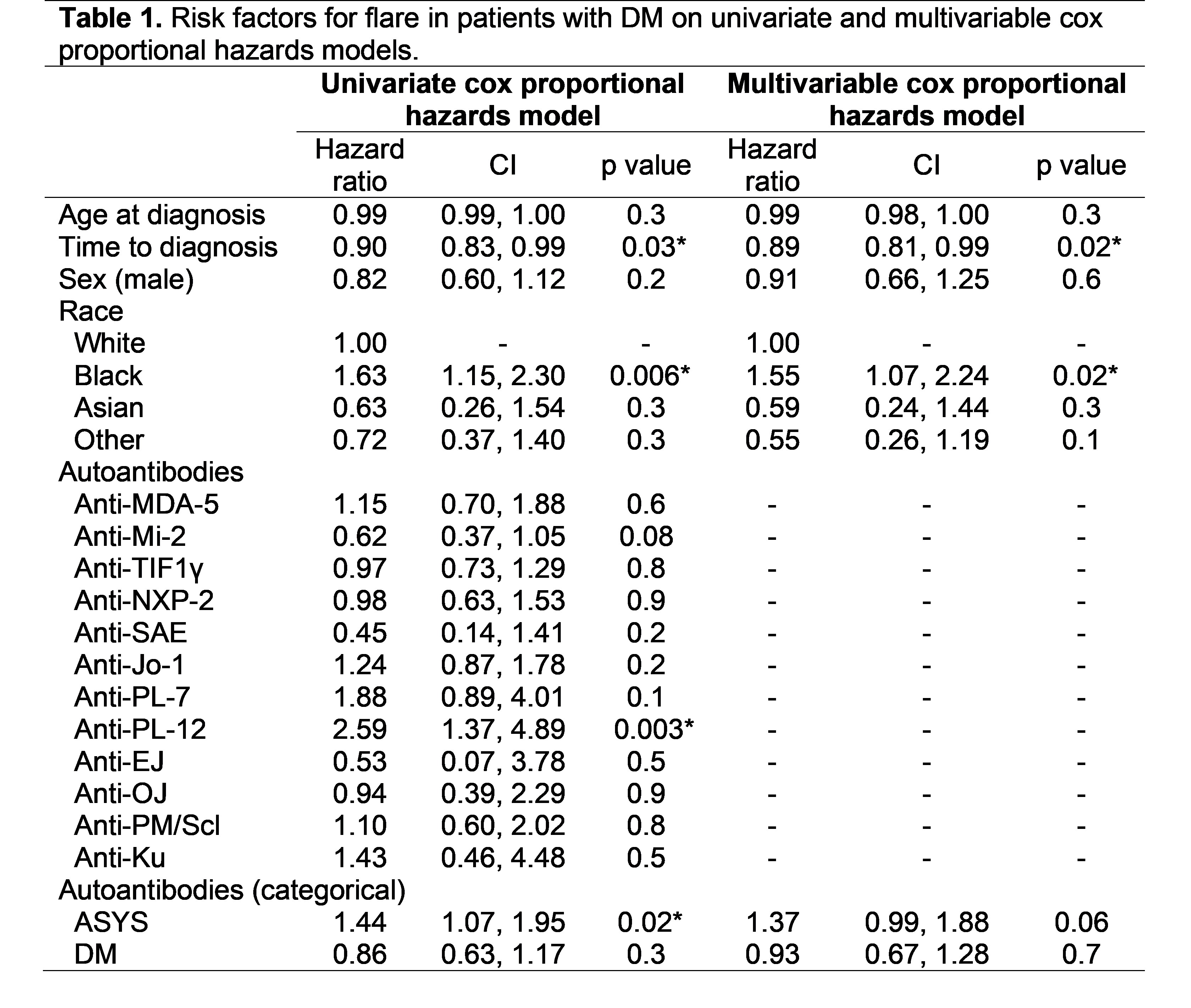
Results: A total of 637 patients with DM (75.4% female; 77.1% White; average age at diagnosis of 48.7 [±13.7]) were included. The patients had an average follow up of 7.9 years (± 4.6), during which time 35.5% (n=226) had at least one flare. Among patients with flare, DM rash documented on exam was the most common finding (75.7%), followed by muscle weakness (58.4%), new/worsening findings on PFTs and/or lung imaging (19.0%) and inflammatory arthritis (12.4%). The majority of the patients who self-reported rash, weakness, dyspnea, joint swelling and dysphagia fulfilled the definition of objective flare (Figure 1). In univariate Cox proportional hazards model, Black race, anti-synthetase (ASYS) autoantibody and shorter time to diagnosis were significantly associated with increased flare risk. On multivariable model, Black race and time to diagnosis remained associated with flare risk (Table 1). Among patients who experienced a flare, the odds of being diagnosed with cancer within 6, 12, or 24 months were significantly lower, suggesting that most flares do not herald a cancer diagnosis. Of the 71 patients diagnosed with cancer after their dermatomyositis diagnosis, 5 (7%) experienced a flare within 6 months of their cancer diagnosis, 8 (11%) within 12 months, and 10 (14%) within 24 months.
Conclusion: In this tertiary care center cohort of patients with DM, approximately one third of the patients experienced at least one flare. Patient-reported symptoms of increased disease activity are often indicative of objective flare. Black race and shorter time to diagnosis were associated with increased risk of flares. Understanding these factors can inform clinicians about timely intervention and improved patient outcomes.
.jpg) Figure 1. Frequency of symptoms reported by patients with DM (A) and proportion of patients who met the objective flare criteria based on self-reported symptom (B).
Figure 1. Frequency of symptoms reported by patients with DM (A) and proportion of patients who met the objective flare criteria based on self-reported symptom (B).
To cite this abstract in AMA style:
Saygin D, Wang Y, Fitzgerald K, Albayda J, Paik J, Tiniakou E, Adler B, Mammen A, Christopher-Stine L, Mecoli C. Predictors and Characteristics of Objective Flares in Adult Dermatomyositis [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/predictors-and-characteristics-of-objective-flares-in-adult-dermatomyositis/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/predictors-and-characteristics-of-objective-flares-in-adult-dermatomyositis/