Session Information
Date: Thursday, March 30, 2023
Title: Poster Breakout 2 - JIA & Uveitis: Genetics, Clinical & Therapeutic Aspects
Session Type: Breakout Session
Session Time: 5:10PM-5:40PM
Background/Purpose: Children diagnosed with oligoarticular juvenile idiopathic arthritis (JIA), the most commonly diagnosed subset of chronic arthritis, are at increased risk of developing uveitis. Known clinical risk factors such as JIA category, ANA positivity, ≤4 years JIA duration, and 6 years old at diagnosis are associated with increased risk but are not definitive. Regular ophthalmic screening is important since uveitis is asymptomatic. Tear fluid biomarkers are easily obtained specimens with great diagnostic potential. In this pilot study, we aim to identify potential tear-based inflammatory markers associated with uveitis development in children with JIA.
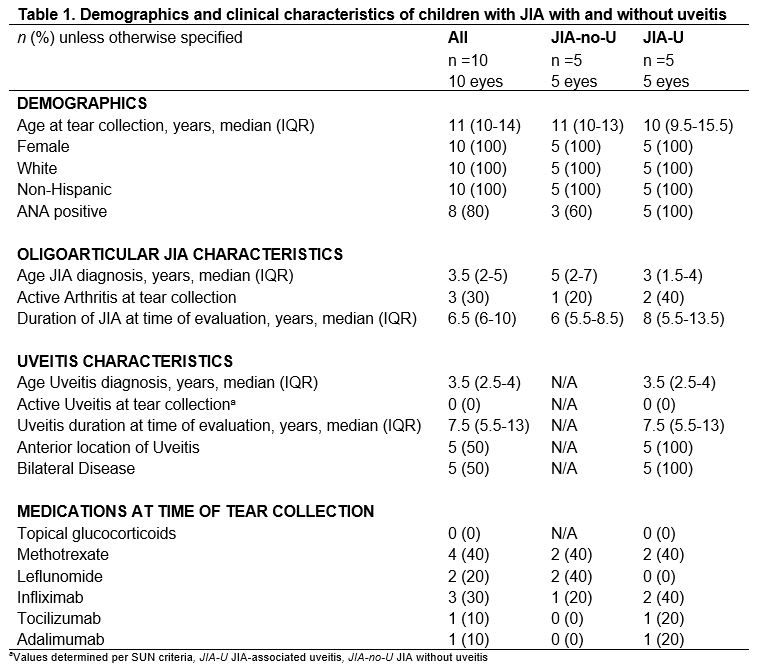
Methods: In this comparative cohort at Cincinnati Childrens with JIA-associated uveitis (JIA-U) and JIA without uveitis (JIA-no-U), participants were enrolled on the basis of high-risk factors: female, non-Hispanic, white and oligoarticular subtype. Medical charts were reviewed for demographics, uveitis characteristics, ophthalmic examination, and current treatment (Table 1). Tear fluid was collected in the left eye using Schirmer strips. We used advanced proteomic strategies (isobaric tag for relative quantitation [iTRAQ] labeling and nanoLC-MS/MS) to quantify and compare proteins in JIA-U and JIA-no-U. A P-value 0.1, based on Wilcoxon rank sum exact test, was considered significant.
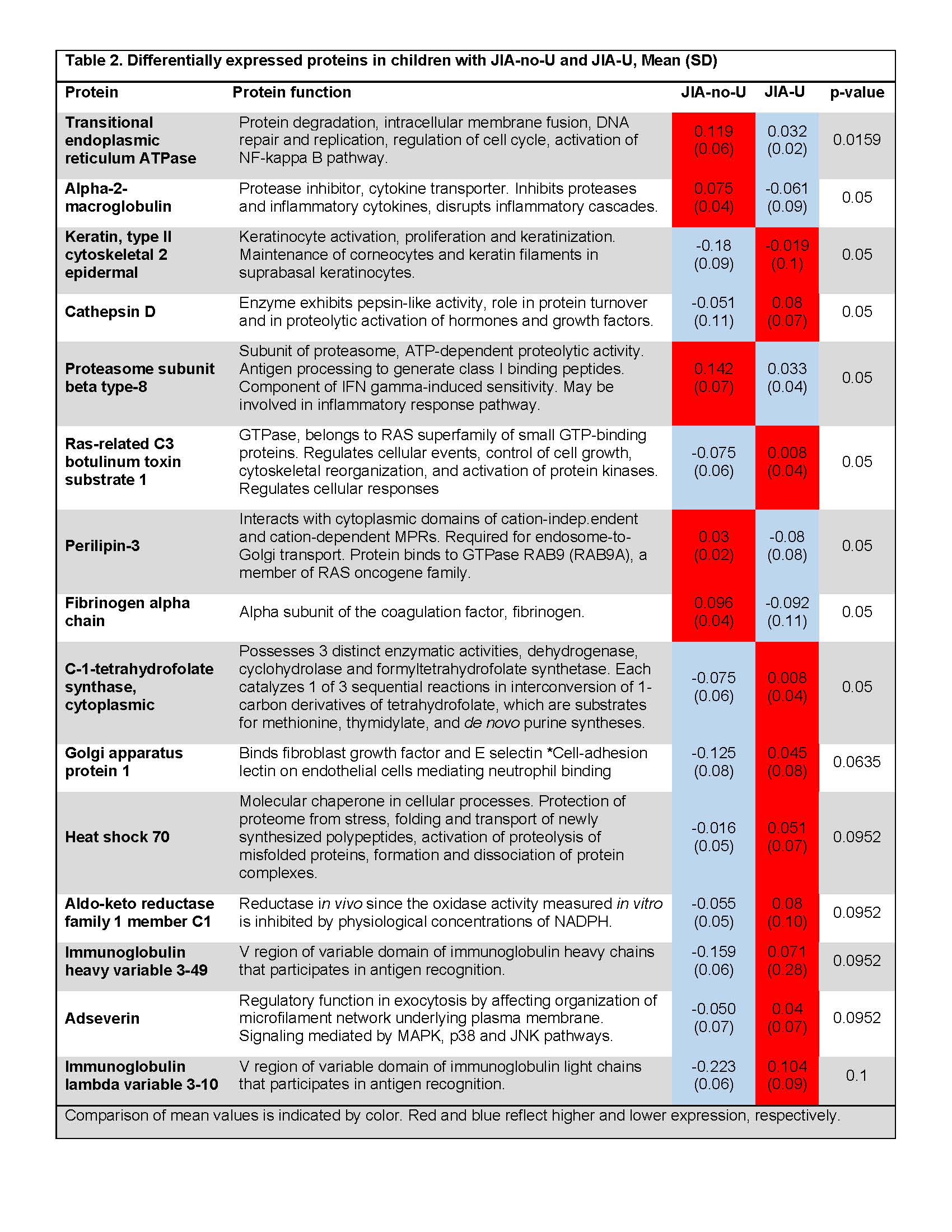
Results: Fifteen proteins exhibited differences in tears of 5 children with JIA-U and 5 with JIA-no-U (Table 2). Of these, 9 showed a difference at p≤0.05. These proteins have been associated with inflammatory arthritis and general inflammatory response pathways. However, Keratin type II cytoskeletal 2 epidermal (KRT2), cathepsin D (CTSD), Ras-related C3 botulinum toxin substrate 1 (RAC1), C-1-tetrahydrofolate synthase, cytoplasmic (MTHFD1), Golgi apparatus protein 1 (GLG1), Heat shock 70 (HSPA1B), Aldo-keto reductase family 1 member C1(AKR1C1), Immunoglobulin heavy variable 3-49 (IGHV3-49), Adseverin (SCIN) and Immunoglobulin lambda variable 3-10 (IGLV3-10 ) demonstrated notably higher expression in tears of those with JIA-U (Table 2). These 10 proteins are associated with the immune response, specifically at the level of retinal pigment epithelium (RPE) and blood retinal barrier (BRB).
Conclusion: Uveitis is a vision-threatening disease that warrants exploration of avenues for early detection and treatment. The eye is an immune-privileged organ, immunologically shielded by the RPE as part of the BRB.Wehypothesize that the immune response proteins identified within the tears of JIA-U patients are byproducts of inflammation-induced RPE and BRB breakdown and furthers the inflammatory cascade. Tears of children with JIA-U and JIA-no-U display differential expression of protein biomarkers that may be a useful clinical source of potential onset of uveitis for those diagnosed with oligoarticular JIA. Furthermore, differential expression of ocular versus joint inflammation may provide insight in the pathogenesis of both JIA and uveitis. Further study in larger cohorts is needed to verify these results.
To cite this abstract in AMA style:
Nguyen T, Maccora I, Altaye M, Haffey W, Hennard T, Sproles A, Thornton S, Miraldi Utz V, Greis K, Angeles-Han S. Potential Uveitic Biomarkers in Tears of Children with Juvenile Idiopathic Arthritis: A Pilot Study [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 4). https://acrabstracts.org/abstract/potential-uveitic-biomarkers-in-tears-of-children-with-juvenile-idiopathic-arthritis-a-pilot-study/. Accessed .« Back to 2023 Pediatric Rheumatology Symposium
ACR Meeting Abstracts - https://acrabstracts.org/abstract/potential-uveitic-biomarkers-in-tears-of-children-with-juvenile-idiopathic-arthritis-a-pilot-study/