Session Information
Date: Tuesday, November 12, 2019
Title: Epidemiology & Public Health Poster III: OA, Gout, & Other Diseases
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: In a seminal BMJ paper (Prior 1986), the Tokelau Island migrant study for gout and hyperuricemia concluded preventive strategies to modify body mass, diet and patterns of alcohol use were needed to prevent gout in this migrant population living in urban New Zealand (9 times higher risk of gout vs. their non-immigrant counterparts). This and other multiple layers of epidemiologic and trial evidence suggesting the importance of obesity epidemics and lifestyle factors, are at odds with a recent BMJ paper (Major et al 2018) about minimal variance explained by isocaloric diets and an accompanying conclusion “Gout is genetic, and ‘drinking too much beer’ has very little influence on serum urate”. To resolve this issue, we examined key modifiable risk factors in relation to the presence of hyperuricemia and estimated the theoretical proportion of hyperuricemia cases that could be prevented through risk factor modification. For comparison, we also estimated the variance explained for the same risk factors, which does not incorporate an exposure’s prevalence in the population.
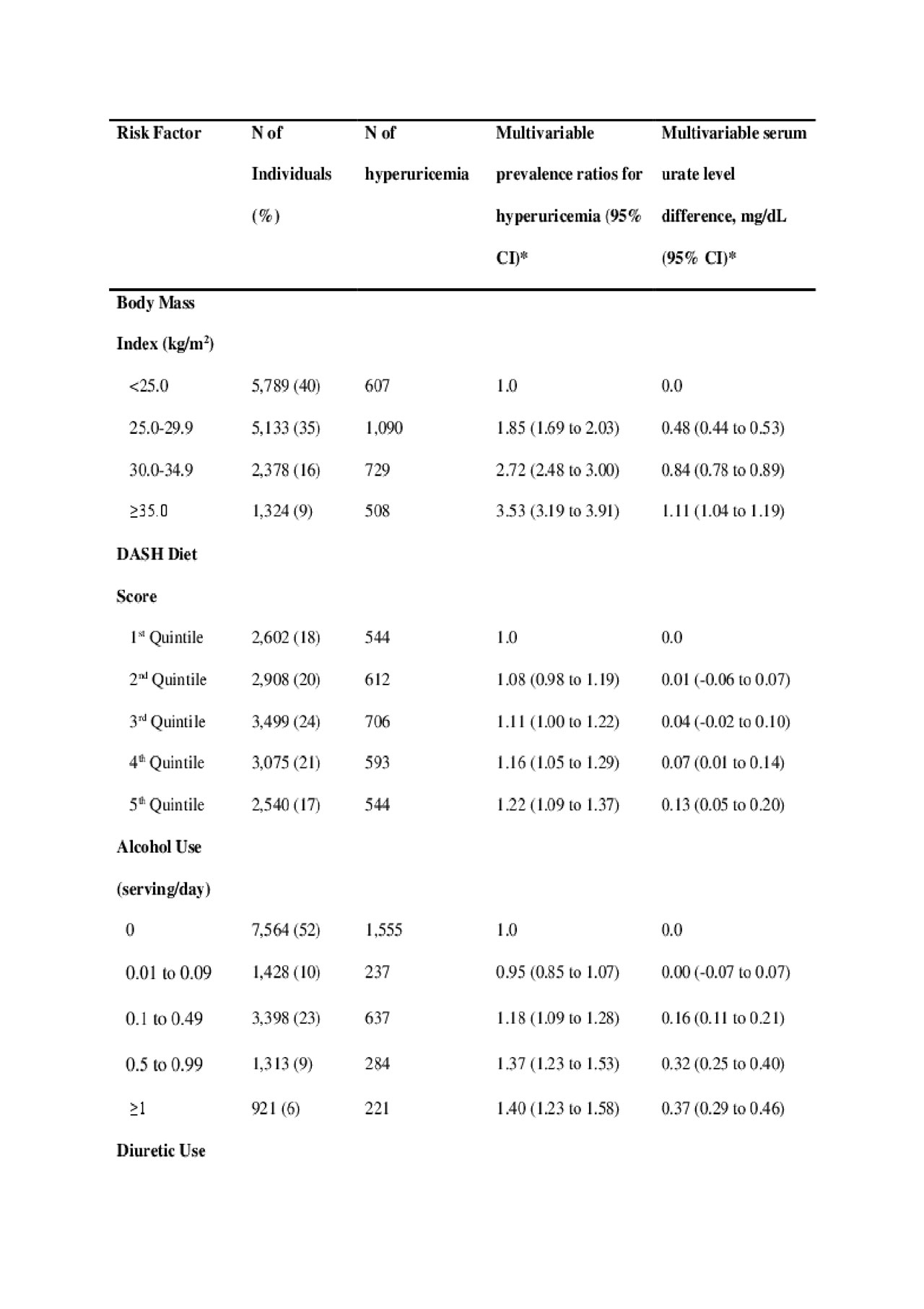
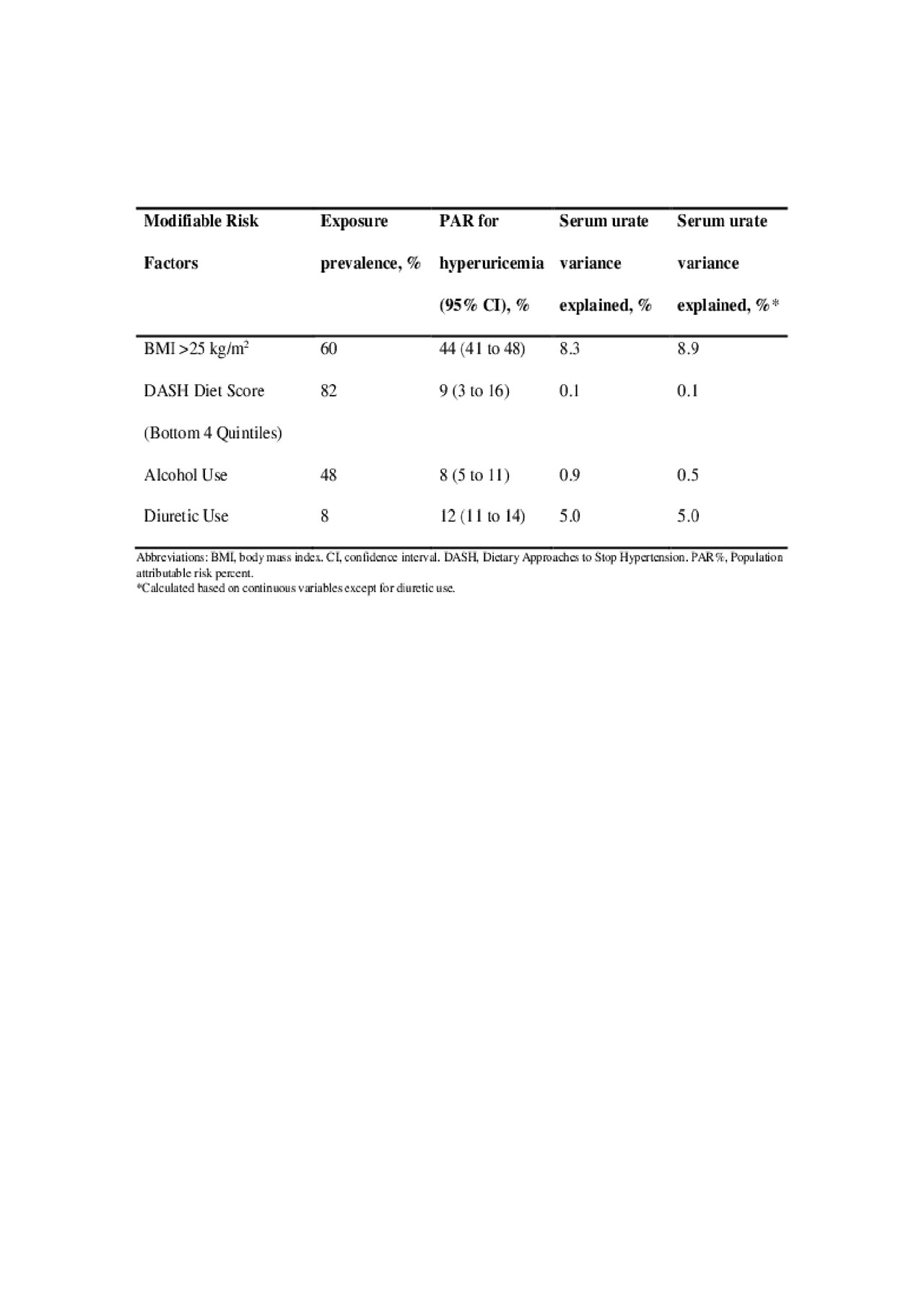
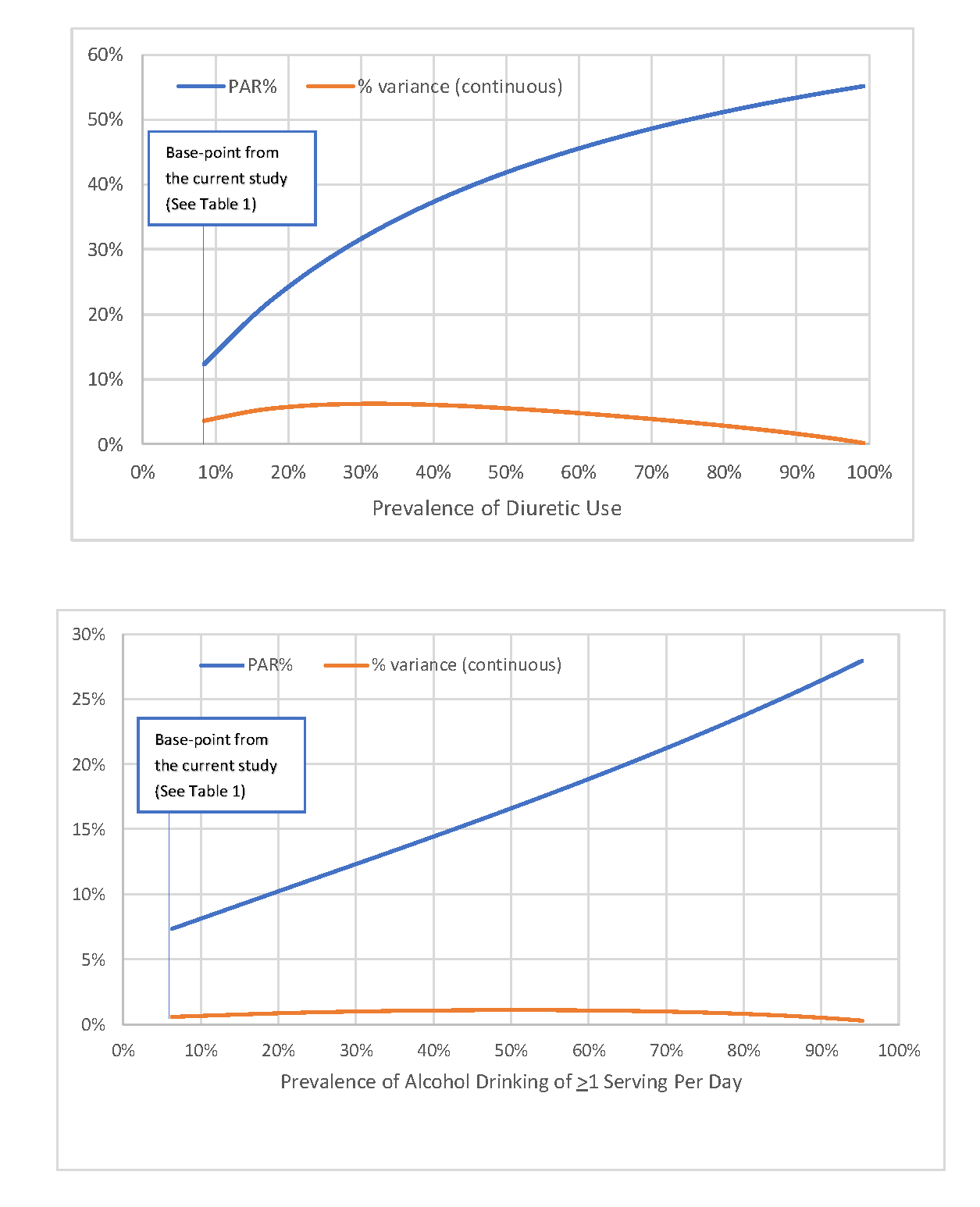
Methods: Using lifestyle, medical and diet data collected in NHANES III, we calculated adjusted prevalence ratios for hyperuricemia, adjusted population attributable risks (PAR) and the variance explained (partial R2 from linear regression models) according to the following four factors: body mass index (BMI ≥25 kg/m2), alcohol intake, non-adherence to a DASH-style diet (bottom 4 quintiles of the DASH diet score) and diuretic use. Hyperuricemia was defined as serum urate > 7.0 mg/dL among men and > 5.7 mg/dL among women. We also conducted simulation analyses to evaluate the impact on PAR and variance explained when varying the prevalence of exposure in the study population.
Results: We included 14,624 adults (mean age 47 years); 20% were hyperuricemic, 60% overweight/obese. BMI, alcohol intake, adherence to DASH-style diet, and diuretic use were all independently associated with serum urate levels and presence of hyperuricemia in a dose-response manner (Table 1). PARs of hyperuricemia cases for overweight/obesity, non-adherence to a DASH-style diet, alcohol use, and diuretic use were 44%, 9%, 8%, and 12%, respectively, while corresponding variances explained were 8.9%, 0.1%, 0.5%, and 5.0% (Table 2). Using the top half, decile and percentile of the DASH diet score as the reference group, PAR%s were 6%, 14% and 40%, respectively. Excluding those with self-reported history of gout or taking hyperuricemia drugs did not materially alter our results, nor did using an alternative definition of hyperuricemia ( > 7.0 mg/dL in both sexes). Our simulation study showed the variance nearing zero with exposure prevalence’s nearing 100% (Figure).
Conclusion: In this national sample of US men and women, four modifiable risk factors (BMI, DASH diet, alcohol use and diuretic use) independently accounted for a large proportion of hyperuricemia cases, suggesting a substantial role for modification intervention. However, the corresponding serum urate variance explained by these risk factors was far smaller and paradoxically masked their high prevalences, providing real-life empirical evidence for its limitations in assessing common environmental risk factors.
To cite this abstract in AMA style:
McCormick N, Lu N, Rai S, Yokose C, Zhang Y, Choi H. Population Impact Attributable to Modifiable Risk Factors for Hyperuricemia and the Fallacy of the Variance Explained [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/population-impact-attributable-to-modifiable-risk-factors-for-hyperuricemia-and-the-fallacy-of-the-variance-explained/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/population-impact-attributable-to-modifiable-risk-factors-for-hyperuricemia-and-the-fallacy-of-the-variance-explained/