Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: The purpose of this study was to pilot test a patient-reported social risk factor (SRF) screening tool among rheumatology outpatients and to examine the distribution of SRFs in patients with autoimmune diseases. It is well documented that adverse social determinants of health can negatively impact patients with autoimmune conditions. Thus, screening patients for SRFs could improve outcomes for patients.
Methods: A SRF screening tool was distributed and completed via the MyChart patient portal of the electronic health record (EHR), a text messaging link on patients’ mobile phones, or iPads in clinic. Patients were screened for four core SRF domains (financial strain, housing instability, food insecurity, transportation needs) and four supplemental SRF domains (physical inactivity, social isolation, stress, depression). Aggregate data from the EHR was extracted for all patients with at least one domain screened and who were seen by a participating rheumatology provider between January 1, 2023 and October 31, 2023. Descriptive statistics of SRFs were calculated. Multivariable logistic regressions were used to examine associations between sociodemographic, clinical characteristics and each SRF.
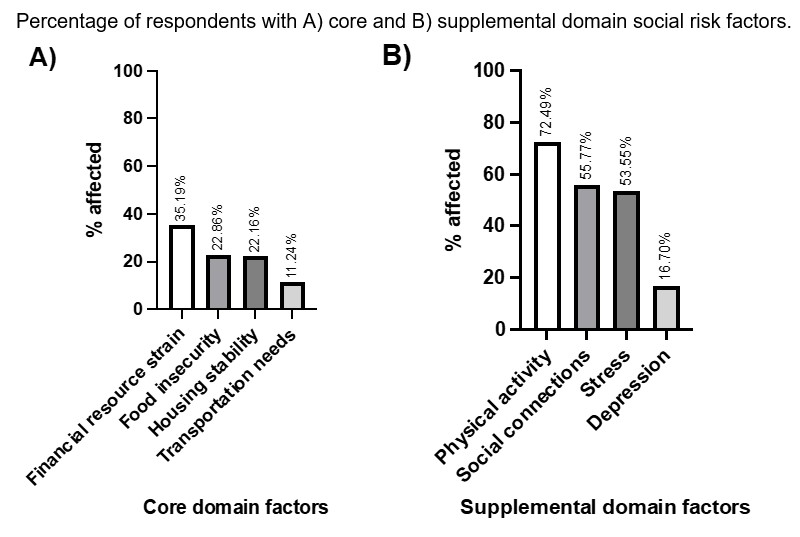
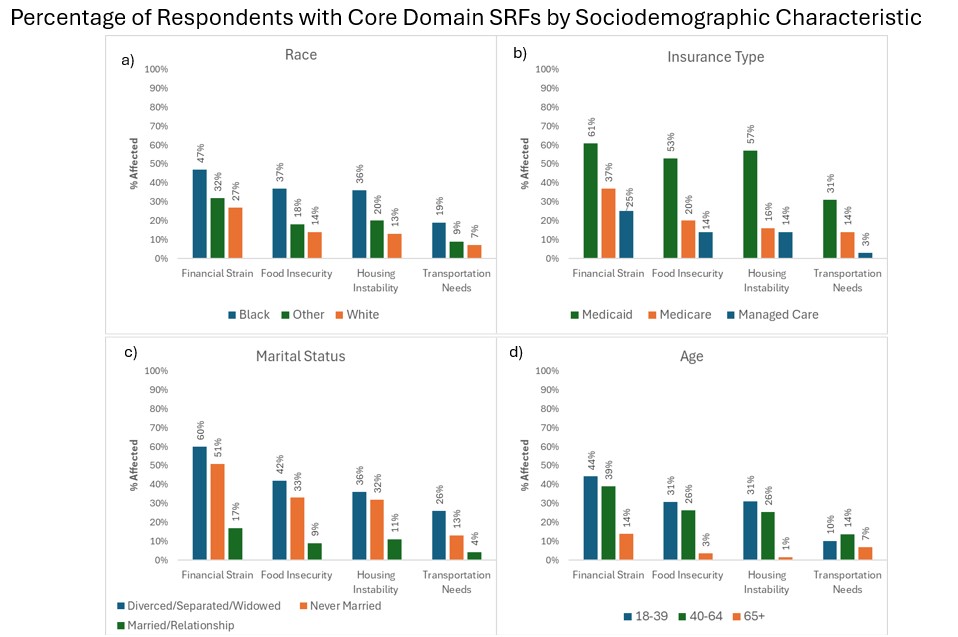
Results: During our initial pilot phase, 148 out of 187 patients were screened (79%). Only three patients outright refused screening. The final analytic sample included 483 individuals with an average age of 50 years old and 84% female (Figure 1). Eighty-four percent of patients screened positive for at least one SRF and the median number of SRFs was 2 (IQR: 1, 4). Physical inactivity (73%, 311/429), and social isolation (58%, 212/367) were the most common SRFs. Among the Core SRF domains, prevalences were 35% for financial strain (145/412), 22% for housing instability (82/370), 23% for food insecurity (96/420), and 11% for transportation needs (48/427) (Figure 2). Patients with Black race, Medicaid insurance, non-married, and younger age had higher reported SRFs than patients with White race, other insurance types, married, and older age respectively (Figure 3). Multivariate analyses showed that Medicaid insurance increased odds of reporting SRFs in all 4 core domains. Black versus White race, was associated with increased odds of reporting food insecurity and housing instability. Primary clinic diagnosis was not associated with increased odds for reporting SRFs.
Conclusion: Our SRF screening program identified a high burden of SRFs among this rheumatology patient population. This study gives a new level of detail into our patients’ barriers and possible needs. It provides immediately actionable data for providers and clinical social workers. This was successfully implemented in several rheumatology clinics using existing EHR tools, and assistance from clinic staff. Future work should seek to uncover associations between SRFs and clinical outcomes, and further interventions to address SRFs should be developed.
To cite this abstract in AMA style:
Chandler A, Hamid M, Jiao A, Hulcher K, Sharma I, Odom P, Robinson A, Kellahan S, Kepper M, Dostal C, Fenelon S, Eisen S, Lew D, Kim A. Patient-reported Social Risk Factor Screening Among Rheumatology Outpatients [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/patient-reported-social-risk-factor-screening-among-rheumatology-outpatients/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/patient-reported-social-risk-factor-screening-among-rheumatology-outpatients/