Session Information
Date: Friday, November 6, 2020
Title: Patient Outcomes, Preferences, & Attitudes Poster I: RA, Spondyloarthritis, & OA
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Time from diagnosis to treatment has been well established to correlate with better outcomes in rheumatoid arthritis (RA). Treatment delays are often associated with worse outcomes and more difficult to treat disease, while early and aggressive treatment leads to better outcomes and increased levels of rheumatoid disease activity (DA) improvement. However time from symptom onset to diagnosis has been less discussed. Building on a collaboration between a non-profit organization and an academic rheumatology center, we aimed to gain greater understanding of the impact of time from symptom onset to diagnosis of RA.
Methods: An anonymous 28-item questionnaire was developed and pilot-tested by the study team and presented in 2019 on a secure online survey system. Eligible participants were U.S. residents age ≥18 years with a self-reported diagnosis of RA by a medical professional. They were asked questions about socio-demographics, RA disease activity, diagnosis and DMARD history, improvement from RA treatment, and RA treatment goals created with their provider. Analyses included descriptive statistics with chi-square and rank sum tests for comparisons.
Results: The questionnaire was completed by 907 self-reported RA patients (90% women, 10% men), with a mean (SD) age of 58 years and a mean of 11.1 (10.1) years since diagnosis. According to patient self-reports, 5% were in remission, 22% reported mild DA, 54% moderate DA, and 19% severe DA.
The longer the time to diagnosis, the more likely people were to report moderate to severe DA levels (< 6mo 65%; >6mo-5yr 75%; >5yr 80%). Similarly, people with a shorter time to diagnosis were twice as likely to reach DA improvement levels ≥70% as those with long times to diagnosis (< 6mo 48%; >6mo-5yr 38%; >5yr 24%).
Longer times from symptom onset to diagnosis also associated with longer times between RA diagnosis and eventual treatment. When the time from symptom onset to diagnosis was < 6 months, time from RA diagnosis to treatment was only an additional 0.8 years. However for those whose diagnosis took >5 years, time from RA diagnosis to treatment initiation was an average of an additional 1.5 years.
The longer the time to diagnosis, the less satisfaction and greater dissatisfaction people with RA had with their rheumatology care (satisfied/very satisfied was reported in: < 6mo 76%; >6mo-5yr 71%; >5yr 65%). Additionally, those describing their health as poor/very poor tended to have longer times to diagnosis (< 6mo 18%; >6mo-5yr 21%; >5yr 27%).
Conclusion: This web-based survey found previously unreported associations between time from symptom onset to RA diagnosis and more severe disease activity and lower responses to treatment, independent of time to between RA diagnosis and treatment initiation. Our study is unique in that time to diagnosis and / or to treatment are reported by patients with RA. Further research should seek greater understanding of the significance of early RA diagnosis and investigate ways to decrease times from symptom onset to RA diagnosis.
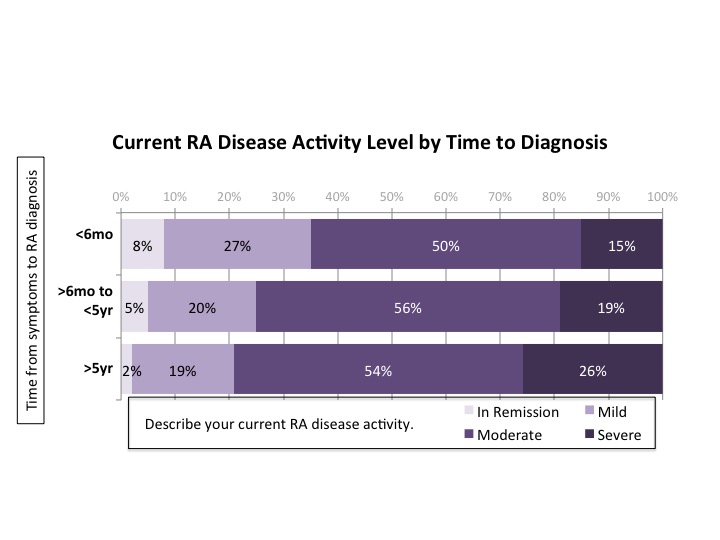 Fig.1 Current RA Disease Activity Level Versus Time to Diagnosis
Fig.1 Current RA Disease Activity Level Versus Time to Diagnosis
 Fig.2 Disease Activity Improvement Level by Time to Diagnosis
Fig.2 Disease Activity Improvement Level by Time to Diagnosis
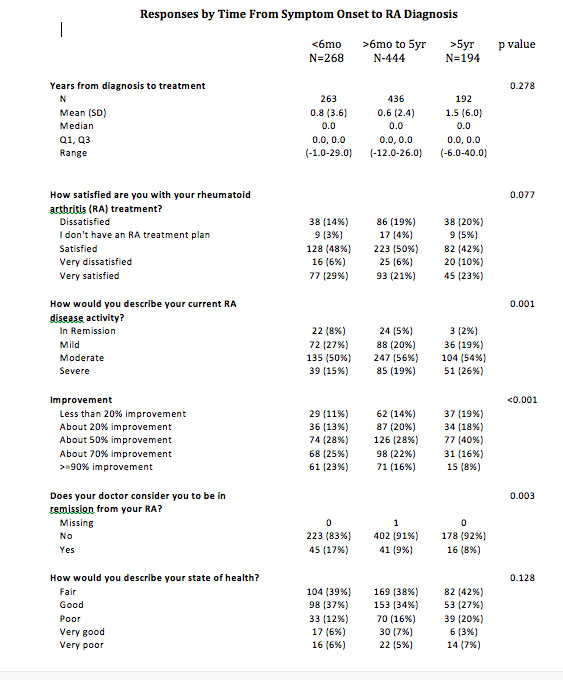 Table1 Responses by Time from Symptom Onset to RA Diagnosis
Table1 Responses by Time from Symptom Onset to RA Diagnosis
To cite this abstract in AMA style:
O'Neill K, Marks K, Davis J, Crowson C. Patient-Reported Data Show the Impact of Time to Diagnosis in RA [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/patient-reported-data-show-the-impact-of-time-to-diagnosis-in-ra/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/patient-reported-data-show-the-impact-of-time-to-diagnosis-in-ra/
