Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Pediatric rheumatic diseases require frequent medical interactions, including follow-up visits with various providers, lab testing, imaging procedures, and infusion treatments. The impact of these conditions extends beyond medical needs, affecting financial, social, educational, and emotional health. Our local pediatric rheumatology clinic implemented a barriers to care assessment in order to identify needs reported by patients and families related to the child’s chronic health condition. The objective of this analysis is to determine the most frequently reported barriers and to assess self-reported medication adherence.
Methods: This is a retrospective analysis of data collected through a local quality improvement initiative. We utilized a modified self-management assessment tool initially developed by the Pediatric Rheumatology Care and Outcomes Improvement Network (PR-COIN). Our local team of multidisciplinary stakeholders including physicians, nurse practitioners, registered nurses, social workers, and parents of pediatric rheumatology patients iteratively adapted PR-COIN’s tool to include a list of 14 financial, social, educational, and emotional barriers most relevant to patients in our setting. We also added a question to assess medication adherence, “I/my child misses a medication dose…”, with 5 Likert response categories from “Never” to “Always”. The forms were available in English and Spanish. All return rheumatology patients were asked to complete the form at the beginning of their clinic visit. We calculated the responses for each barrier category and organized the responses from most to least frequently reported. We also calculated the number of responses to each medication adherence category.
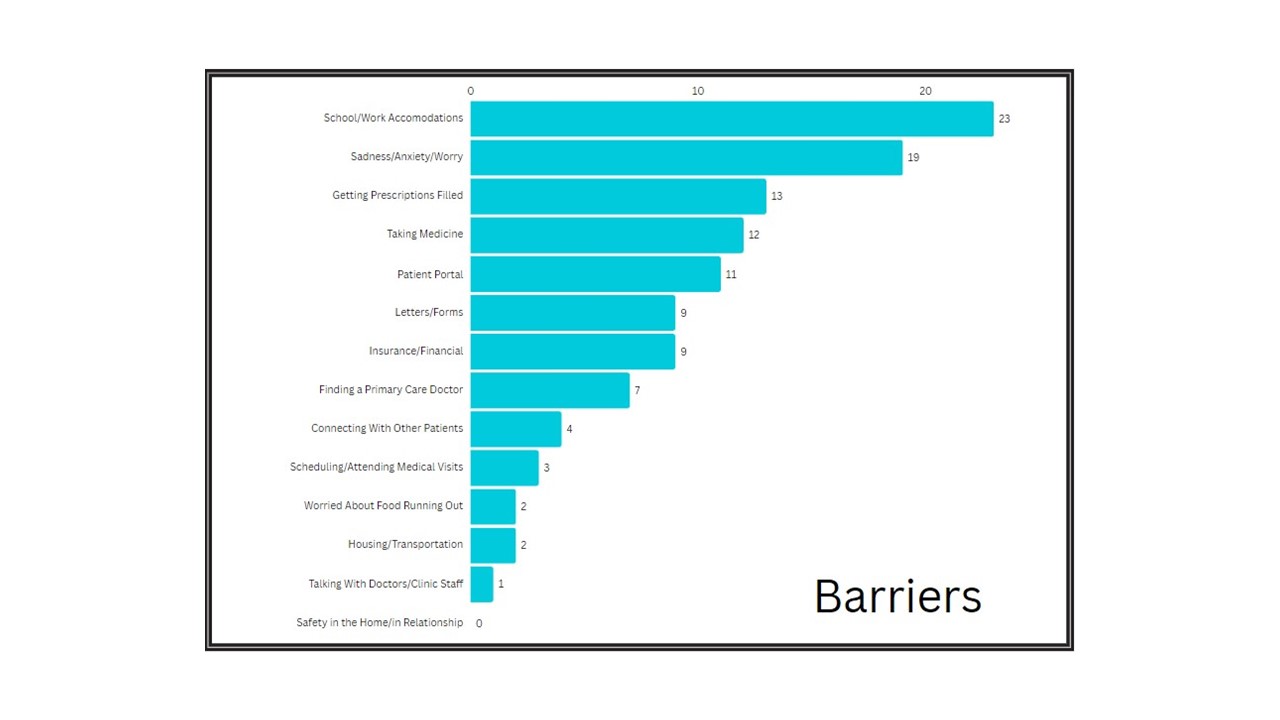
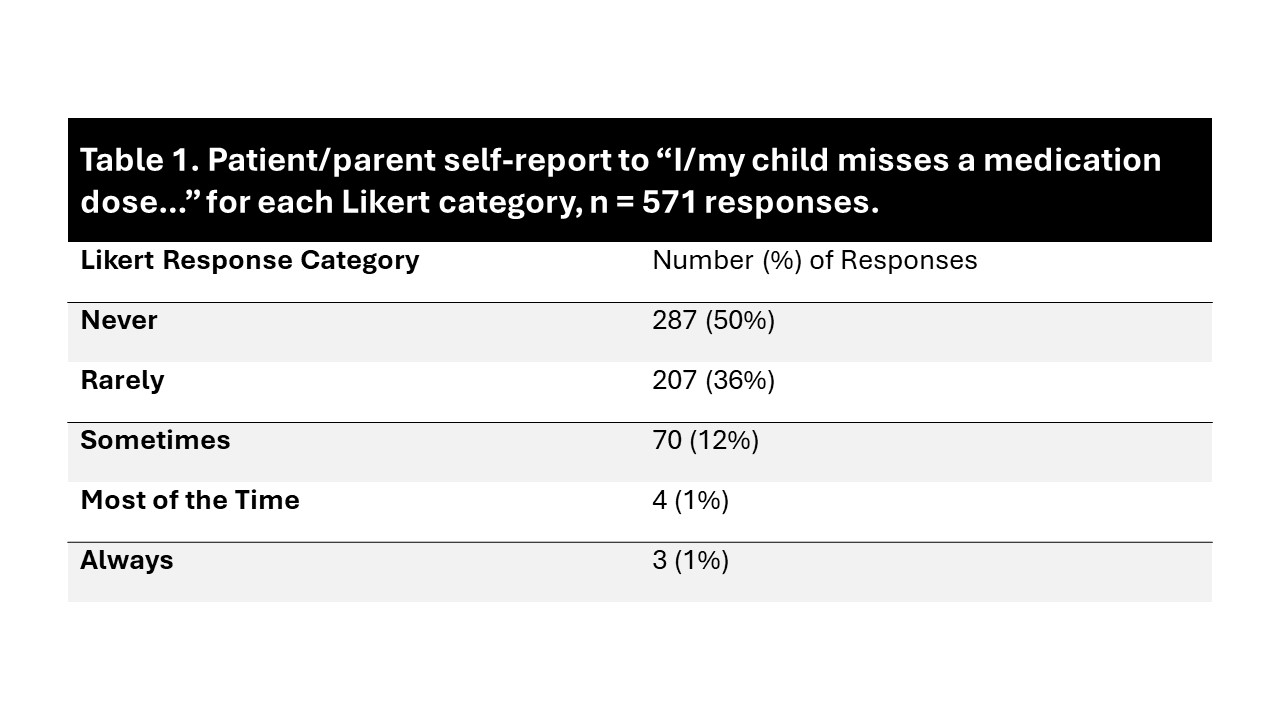
Results: From 2022 until 2024, we collected patient/parent responses from 591 visits. There were a total of 114 barriers identified; arranged from most to least frequent, the identified barriers were (% of total barriers): school/work accommodations (20%), sadness/anxiety/worry (17%), getting prescriptions filled (11%), taking medicine (11%), patient portal (10%), insurance/financial (8%), letters/forms (8%), finding a primary care doctor (6%), connecting with other parents (4%), scheduling/attending medical visits (3%), worried about food running out (2%), housing/transportation (2%), and talking with doctors/clinic staff (1%) (Figure 1). Additionally, 50% of patients reported never missing medication doses, 36% reported rarely, 12% reported sometimes, 1% reported most of the time, and 1% reported always (Table 1).
Conclusion: After reliably implementing a barriers to care assessment in our local pediatric rheumatology clinic, we identified the most frequently reported barriers were related to school and work as well as mental health. Relatively few patients/parents reported missing medications more often than rarely. This initial data provides insight on the barriers faced by our pediatric rheumatology patients and families. Future work will be able to focus on additional interventions for the most frequently identified barriers and further study gaps in resources to meet those needs.
To cite this abstract in AMA style:
Walker B, Smith C, Bridges J, McAllister L, McCamy A, Reed A, Reynolds E, Robles I, Timmerman L, Webb T, Mannion M, Smitherman E. Patient-Reported Barriers to Care Across Pediatric Rheumatology Patients at a Tertiary Academic Medical Center [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/patient-reported-barriers-to-care-across-pediatric-rheumatology-patients-at-a-tertiary-academic-medical-center/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/patient-reported-barriers-to-care-across-pediatric-rheumatology-patients-at-a-tertiary-academic-medical-center/