Session Information
Date: Monday, October 27, 2025
Title: (1248–1271) Patient Outcomes, Preferences, & Attitudes Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Patients with rheumatic diseases face complex and chronic diagnoses that require close monitoring and frequent communication with their providers. Given increasing challenges to in-person medical care, including decreased time for clinic visits, physician shortages, and scheduling difficulties, online patient portals serve as important tools to engage patients in their care, allowing them to review test results, schedule appointments, and communicate with physicians. To identify barriers to portal use, we evaluated rheumatology patients’ awareness, use, and perceptions of patient portals across three clinical sites: a public safety net hospital, private academic teaching hospital and Veterans Affairs (VA) Hospital.
Methods: We conducted a cross-sectional, survey-based study in outpatient adult rheumatology clinics in three hospitals. During routine visits, surveys were distributed to patients in English or Spanish. Surveys assessed demographics, educational background, familiarity with each hospital system’s portal, frequency and reason for portal use, and interest in learning more. Informational handouts on portal capabilities and sign-up instructions were provided.
Results: 139 patients completed the survey: 50 from the VA, 15 from the private hospital and 74 from the public hospital. The average age was 53.1; 48.2% of respondents were male. Hispanic identity (46.8%) was most common. English was the primary language for 77%. The most reported highest education level was high school (Table 1).93.5% of all patients surveyed were aware of their patient portal, and 71.9% reported using their portal at least once a month. Portal awareness and use declined with age: patients 65 and over were less likely to have internet access or use portals, including a plurality who never used them (Figure 1). Older patients also reported more difficulty navigating portals (Figure 2A). Use varied by hospital, with highest use at the public hospital and lowest at the VA (Figure 2B). At the public hospital, higher educational attainment was associated with increased computer and internet access, whereas computer and internet access were nearly universal at the private hospital, regardless of education.
Conclusion: While awareness of patient portals was high across all sites, actual use was far lower and varied by age and hospital site. Patients 65 and over had the lowest frequency of use, which may be related to reduced access to technology and less favorable attitudes towards portals. Internet and computer access was not universal and varied with educational level, suggesting that access may be a limiting factor. Our findings highlight the need for targeted interventions, such as educational and technical support, as well as alternative communication strategies in those who are unable to utilize patient portals. These efforts would help to increase patient engagement in their medical care, ultimately improving outcomes in rheumatology.
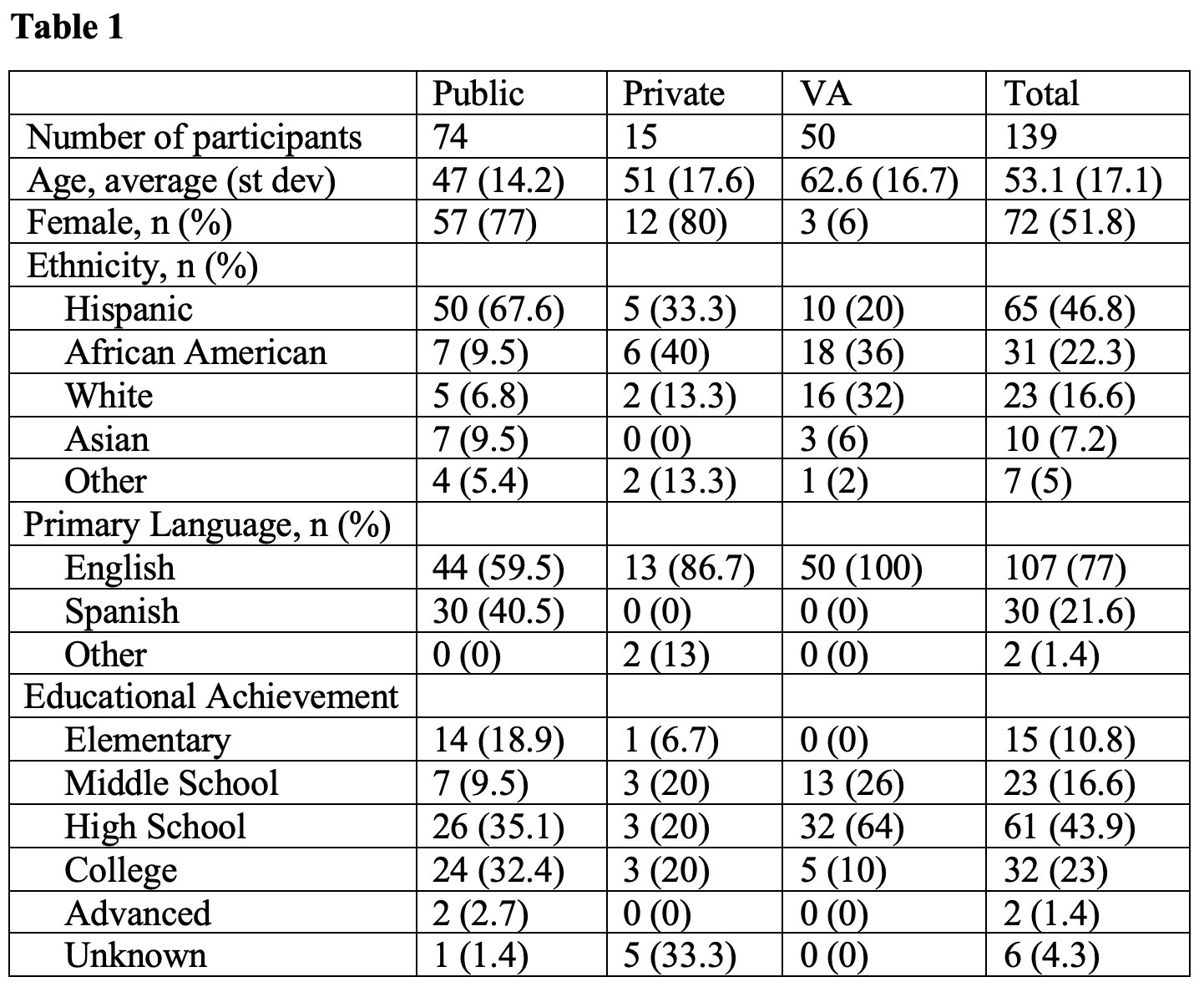 Table 1. Demographic characteristics of survey respondents.
Table 1. Demographic characteristics of survey respondents.
.jpg) Figure 1. Awareness (A) and use frequency (B) of patient portal by age. Answers for panel A refer to “I am aware of my patient portal.”
Figure 1. Awareness (A) and use frequency (B) of patient portal by age. Answers for panel A refer to “I am aware of my patient portal.”
.jpg) Figure 2. Difficulty using patient portal by age (A) and portal usage by health system (B). Answers refer to “I have trouble using my patient portal” and “I find my patient portal useful for my needs.”
Figure 2. Difficulty using patient portal by age (A) and portal usage by health system (B). Answers refer to “I have trouble using my patient portal” and “I find my patient portal useful for my needs.”
To cite this abstract in AMA style:
Gutowski E, Novack J, Covello A, Carlucci P, Goldberg S, Guan M, Hines M, Philips E, Pillinger M, Stream S. Patient Portal Awareness and Utilization Across Diverse Rheumatology Populations [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/patient-portal-awareness-and-utilization-across-diverse-rheumatology-populations/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/patient-portal-awareness-and-utilization-across-diverse-rheumatology-populations/
