Session Information
Session Type: Poster Session B
Session Time: 8:30AM-10:30AM
Background/Purpose: Although pain is one of the most common and highest priority symptoms reported by people with autoimmune inflammatory myopathies (AIM), large descriptive studies on pain in AIM are lacking. The objective of this study was to assess the prevalence, severity, functional impact, and clinical correlates of pain in AIM.
Methods: We undertook a cross-sectional study of adult AIM subjects in a large multicenter cohort. Standardized clinical histories, medical examinations, and self-administered questionnaires were collected at baseline study visit. Severity of pain was assessed using a Numeric Rating Scale (NRS; scores ranging from 0 (no pain) to 10 (very severe pain)). Pain interference with work (including both work outside the home and housework) was measured using the Short Form 36 (SF-36) (5-point Likert scale: not at all, a little bit, moderately, quite a bit, extremely). Global and skin disease activity were rated by the study physician using a NRS ranging from 0 (no activity) to 10 (maximum severity). Physical functioning was assessed using the Health Assessment Questionnaire (HAQ; scores ranging from 0 (no disability) to 3 (severe disability)). Ordinal logistic regression models were generated to determine the association between pain severity at baseline and selected clinical predictors.
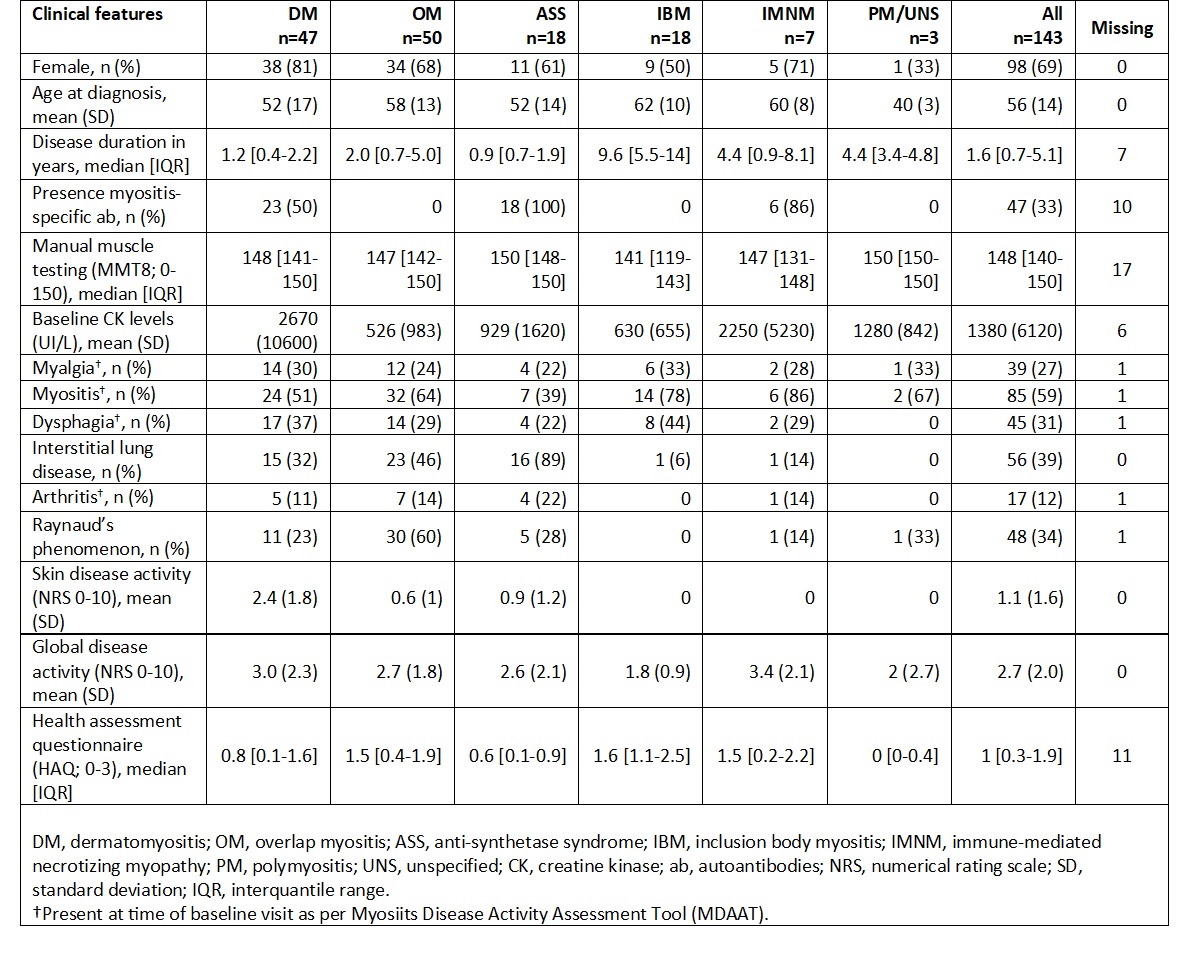
Results: The study included 143 AIM subjects (69% female, median disease duration 1.6 years and mean age at diagnosis 56 years) with dermatomyositis (DM; 33%), overlap myositis (OM; 35%), anti-synthetase syndrome (ASS; 13%), inclusion body myositis (IBM; 13%), immune-mediated necrotizing myopathy (IMNM; 5%), and polymyositis/unspecified (PM/UNS; 2%) (Table 1). At baseline, 27% of subjects had myalgia, 59% active myositis, 39% interstitial lung disease, 12% arthritis and 34% Raynaud’s phenomenon (Table 1). At baseline, mean (SD) skin activity was 1.1 (1.6), and mean (SD) global disease activity 2.7 (2.0). Mean (SD) creatine kinase (CK) was 1380 UI/L (6120). Median (IQR) HAQ score was 1 (0.3-1.9) indicating moderate functional disability.
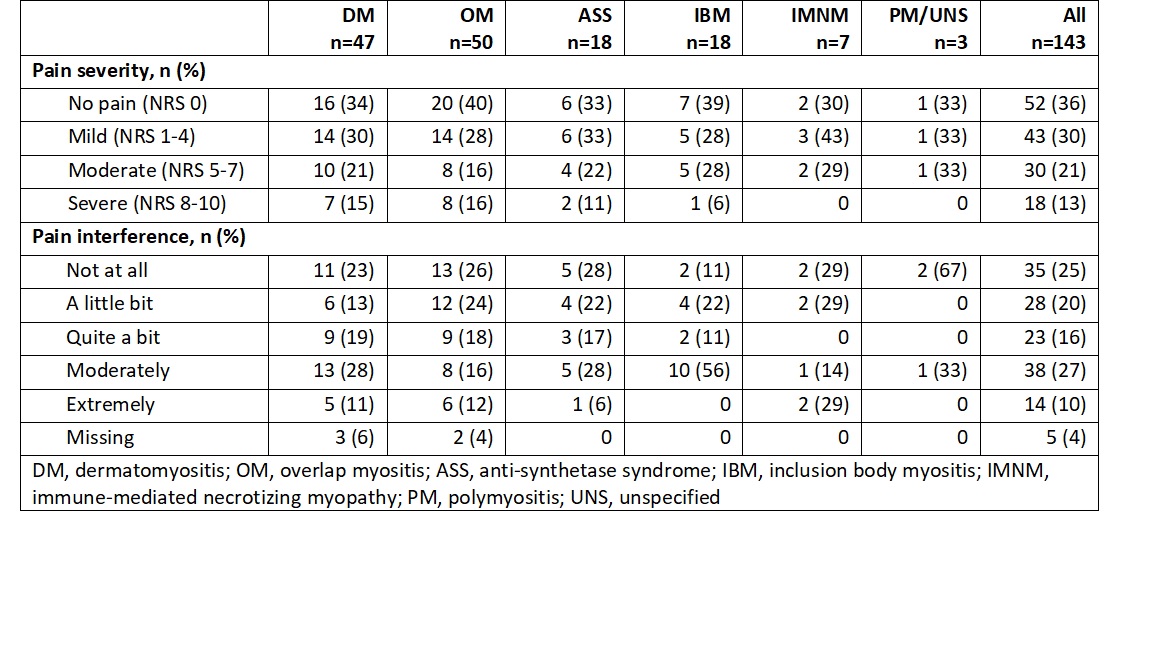
Median (IQR) pain severity was 3 (1-7), with 64% of subjects reporting some level of pain (13% severe, 21% moderate, 30% mild pain) (Table 2). Pain interference with work affected 73% of patients (10% extremely, 27% moderately, 16% quite a bit, 20% a little bit). Among the AIM subsets, a higher percentage of patients with DM, OM, and ASS reported severe pain compared to other subsets. The IBM subjects reported more severe pain interference than in any other subset.
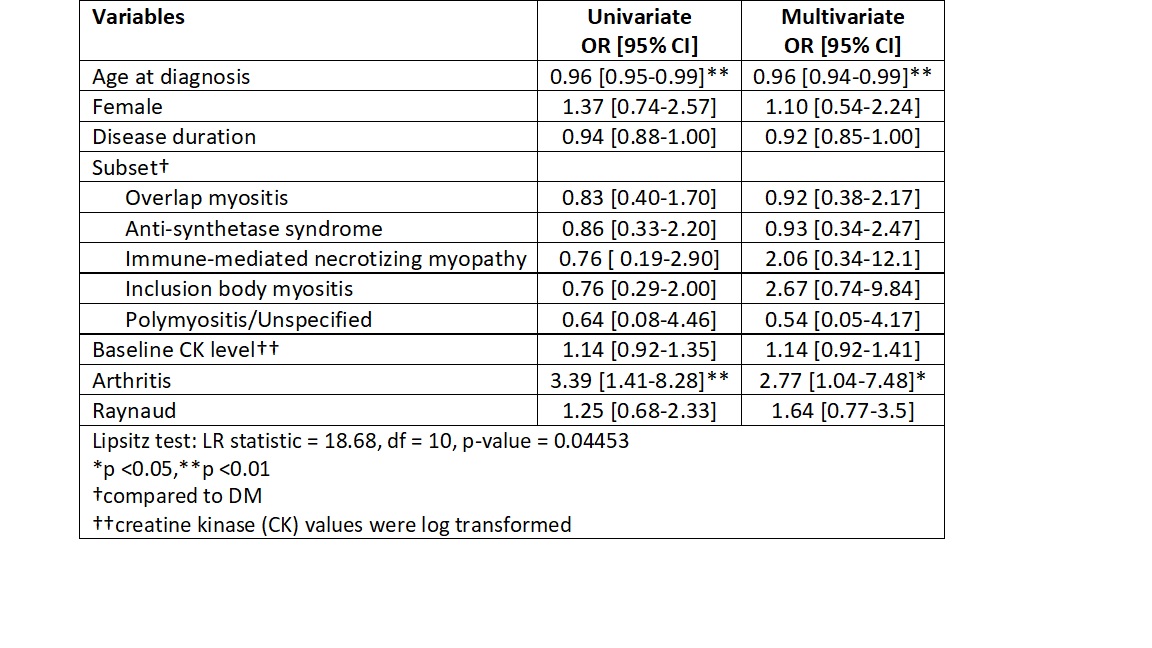
Univariate and multivariate logistic ordinal regressions showed statistically significant associations of baseline pain severity with age at diagnosis and arthritis (Table 3). After adjustment, patients with arthritis were almost 3 times more likely to report higher pain level than those without (OR [95%CI] 2.77 [1.04-7.48], p-value 0.04). By contrast, for every one-year increase in age at diagnosis, the odds of having pain decreased by 4% (OR [95%CI] 0.96 [0.94-0.99], p-value 0.008).
Conclusion: Pain is highly prevalent in adult AIM and interferes with work in 73% of subjects. Further research on correlates and trajectories of pain are urgently needed to inform effective management of pain in AIM.
To cite this abstract in AMA style:
Tsui H, Wang M, Piché M, Ladouceur A, Vinet E, Albert A, Larche M, Tisseverasinghe A, Hudson M, Leclair V. Pain Severity and Interference in Adult Autoimmune Inflammatory Myopathies [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/pain-severity-and-interference-in-adult-autoimmune-inflammatory-myopathies/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/pain-severity-and-interference-in-adult-autoimmune-inflammatory-myopathies/