Session Information
Date: Monday, November 8, 2021
Session Type: Poster Session C
Session Time: 8:30AM-10:30AM
Background/Purpose: Pachymeningitis is a rare disorder defined by localized or generalized inflammatory thickening of the dura. It can be associated with infections, malignancy, autoimmune disorders, or can be idiopathic. The clinical presentation is dependent on the location of dural involvement and regional structures affected. Typical symptoms include chronic headaches, seizures, facial pain, ataxia, and cranial neuropathies. Case series have reported clinical characteristics and outcomes in patients with pachymeningitis; however, large series are lacking. In our retrospective study, we report the clinical presentation, demographics, etiology, imaging features, laboratory data, treatment, and outcome in 153 patients with pachymeningitis referred to our tertiary care center.
Methods: Medical records for all patients with pachymeningitis between 01/01/1990 and 11/01/2019 at our institution were reviewed. Pachymeningitis was defined as focal or diffuse dural thickening or enhancement on magnetic resonance imaging (MRI) of the brain or spinal cord and/or characteristic inflammation on histologic analysis of dura mater tissue samples. Clinical features, laboratory data, radiologic features, pathological findings, and therapeutic data were studied.
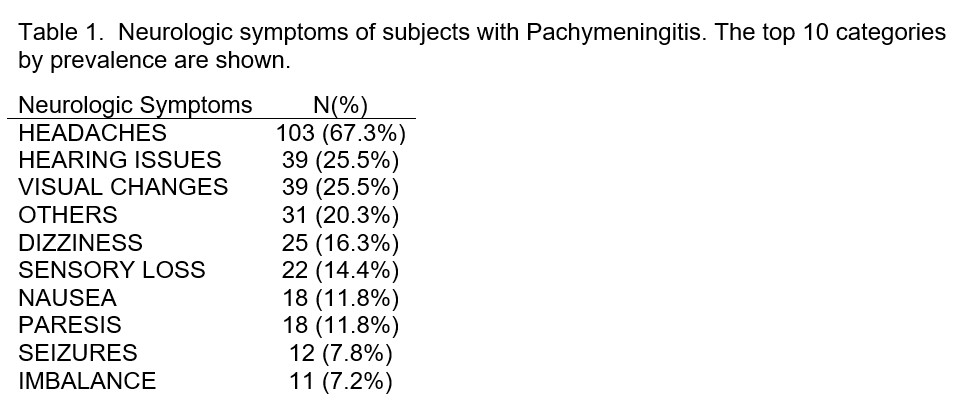
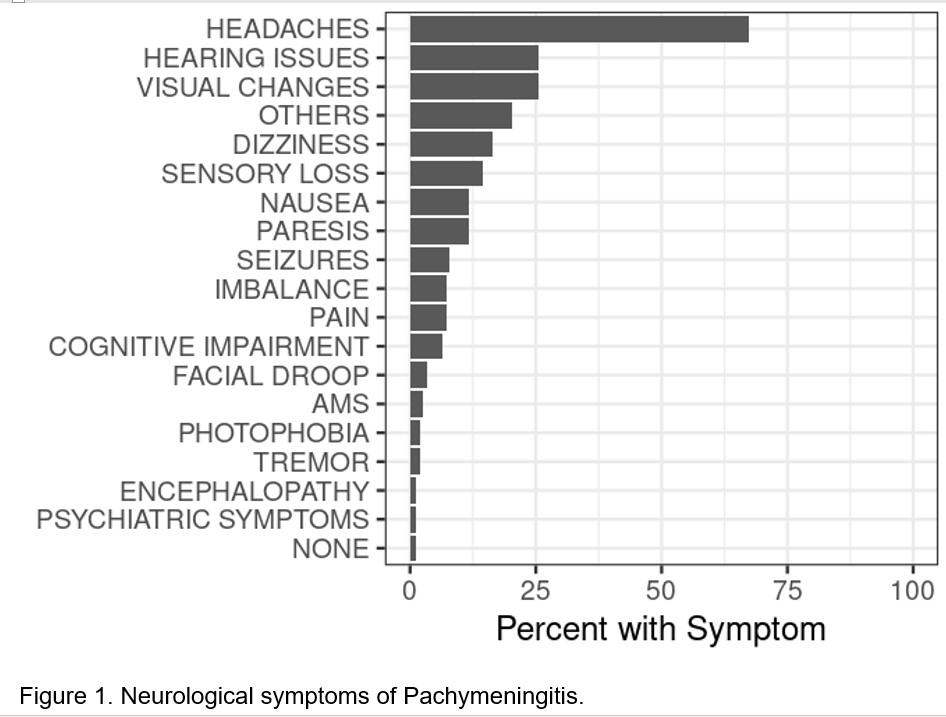
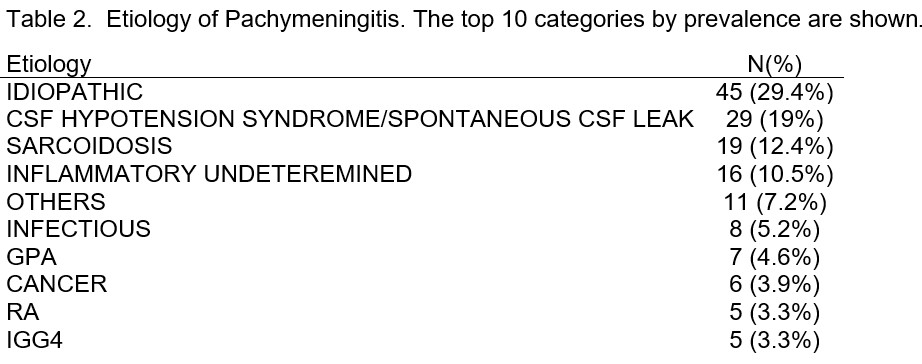
Results: 163 cases of potential pachymeningitis were examined, and 10 patients were excluded for not meeting pachymeningitis definition. The cases were 52.3% female (80/153) and 47.7% male (73/153). Mean age at diagnosis was 60 years (range 21 to 87) with mean age at onset of symptoms 58 years (range 17 to 87). Nearly all patients (98.7%) experienced at least one neurological symptom with headache being the most prevalent (N=103/67.3%; Table 1 and Figure 1). CSF analysis via lumbar puncture was performed in 118 patients with opening pressure being high in 19 of 90 patients. Dural thickening and enhancement was more common on MRI than either radiological finding alone, 56.2% versus 3.9% dural thickening alone or 37.9% enhancement alone (without dural thickening). The majority of cases presented with diffuse pachymeningitis on MRI (62.1%). Biopsy of the cranial or spinal parenchyma or meninges was performed in 42.5% (65/153). Etiology of pachymeningitis was idiopathic in 29.4% (45/153). The top 10 categories of etiology by prevalence are shown in Table 2. 60.1% of patients (92/153) received at least one therapeutic agent. 51.6% of cases received treatment with corticosteroids. Other treatments depending on etiology of the pachymeningitis included methotrexate, blood patch, antimicrobial therapy, rituximab, and azathioprine with highest prevalence. Complete clinical response and complete initial radiologic response were observed in 12.4% (19/153).
Conclusion: We report the largest series of pachymeningitis patients to date. Etiology may be idiopathic or secondary to infections, malignancy, or autoimmune disorders; therefore, appropriate workup is necessary to guide treatment strategy. Limited number of patients demonstrate complete clinical response.
To cite this abstract in AMA style:
Gilbert E, Al-Awqati M, Gunderson T, Berianu F. Pachymeningitis: The Mayo Clinic Experience [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/pachymeningitis-the-mayo-clinic-experience/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/pachymeningitis-the-mayo-clinic-experience/