Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: High maternal body mass index (BMI) is a well-established modifiable risk factor for adverse pregnancy outcomes (APO) in the general obstetric population. Best practices recommend appropriate pre-pregnancy weight management to optimize outcomes. However, the prevalence of obesity and its impact in systemic lupus erythematosus (SLE) pregnancies are poorly understood, despite the higher APO risk in SLE. We evaluated baseline BMI in a prospective SLE pregnancy cohort to determine if overweight (25-29.9 kg/m²) or obese (≥30 kg/m²) BMI conferred higher APO risk compared to BMI < 25 kg/m2.
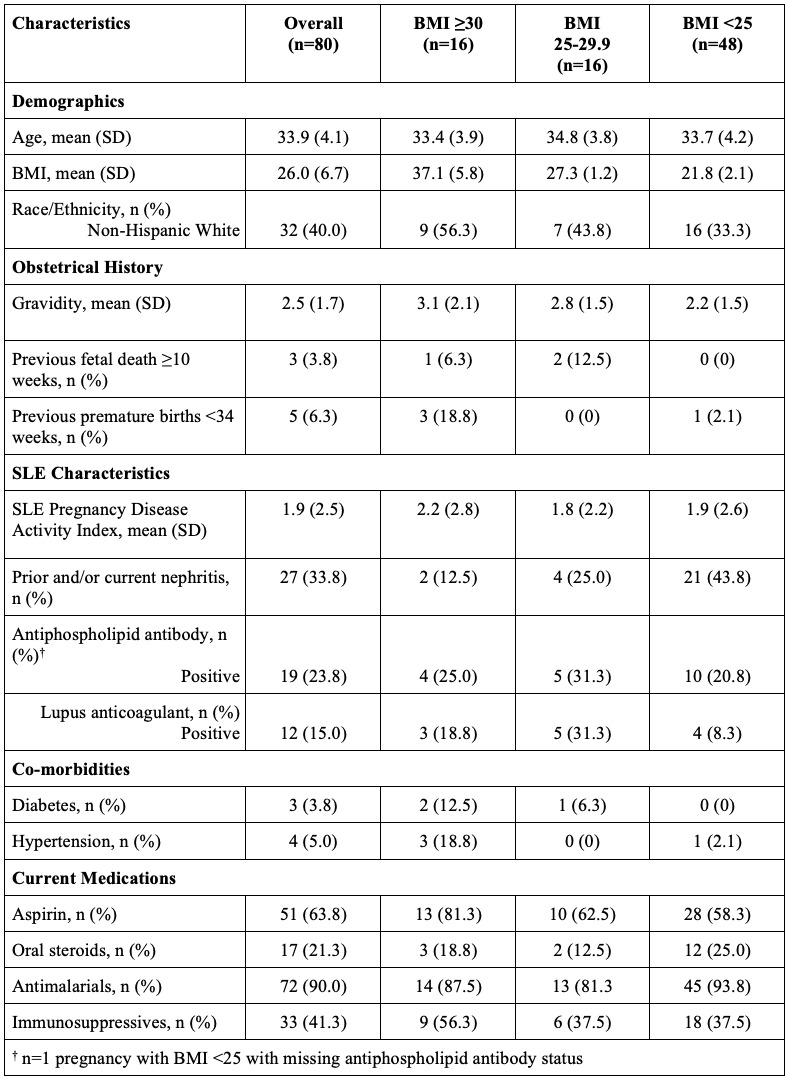
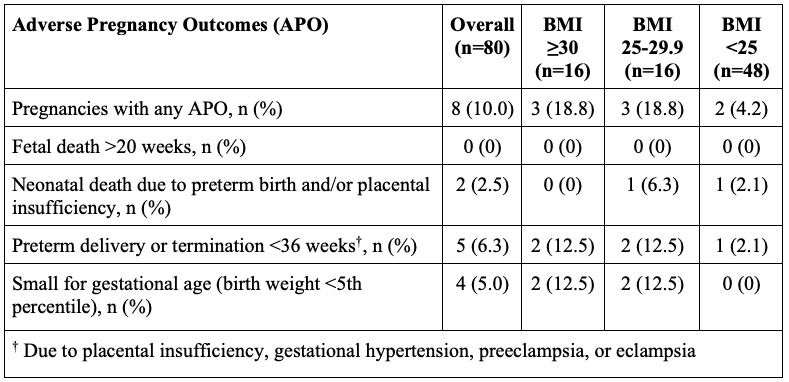
Methods: We enrolled pregnant SLE women at < 17 weeks gestation at Systemic Lupus International Collaborating Clinics (SLICC) centres in Canada (Montreal, Quebec City, Calgary, Halifax) and South Korea (Seoul). We collected data on demographics, obstetrical history, SLE characteristics, baseline co-morbidities, and APO at each of the 2nd trimester, 3rd trimester, and end-of-pregnancy visits (8-12 weeks after end of pregnancy). APO included 1) fetal death >20 weeks gestation, 2) neonatal death due to preterm birth and/or placental insufficiency, 3) preterm delivery or termination < 36 weeks due to placental insufficiency, gestational hypertension, preeclampsia, and/or eclampsia, and 4) small for gestational age (SGA; < 5th percentile). We assessed the proportion of APO across the different BMI groups. We conducted a multivariate analysis using the Korean BMI classification for pregnancies from Asian mothers, categorizing BMI as follows: obese (BMI ≥25), overweight (BMI 23-24.9), and normal weight (BMI < 23).
Results: We analyzed 80 completed pregnancies, with a mean maternal age of 33.9 years (standard deviation, SD 4.1) and a mean maternal BMI of 26.0 kg/m2 (SD 6.7). Almost half (40%) of pregnancies had a maternal BMI ≥25 kg/m2. Non-Hispanic Whites made up 40% of the pregnancies and more than half (56%) of pregnancies with a maternal BMI ≥30 kg/m2 (Table 1). Aspirin use was more common in the BMI ≥30 kg/m2 group, while steroids were more frequently used in pregnancies with BMI < 25 kg/m2. Overall, APO occurred in 8 (10%) pregnancies (Table 2). The proportion of APO was 19% [95% confidence interval (CI) 0, 38%] in both the BMI 25-29.9 kg/m2 and BMI ≥30 kg/m2 groups and 4% (95% CI 1, 12%) in the BMI < 25 kg/m2 group. In univariate analysis, there was more than a 5-fold increased risk of APO in pregnancies with maternal BMI ≥25 kg/m2 versus those with BMI < 25 kg/m2 [odds ratio (OR) 5.31; 95% CI 1.00, 28.24]. In multivariate analysis, using the Korean BMI classification for all Asian mothers, as well as adjusting for race and antiphospholipid antibody status, overweight and obese pregnancies had a substantially increased risk of APO compared to those with normal weight (OR 6.32; 95% CI 1.25, 32.0).
Conclusion: Overweight and obese SLE women had a higher risk of APO compared to the normal weight group. High BMI may be a modifiable risk factor for APO in women with SLE. Preconception weight interventions may improve outcomes in SLE pregnancies.
To cite this abstract in AMA style:
Boivin J, Sacre K, Bernatsky S, Clarke A, Barber M, Fortin P, Hanly J, Legge A, Bae S, Vinet E. Overweight and Obesity Are Key Modifiable Risk Factors for Adverse Outcomes in SLE Pregnancies [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/overweight-and-obesity-are-key-modifiable-risk-factors-for-adverse-outcomes-in-sle-pregnancies/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/overweight-and-obesity-are-key-modifiable-risk-factors-for-adverse-outcomes-in-sle-pregnancies/