Session Information
Date: Tuesday, November 19, 2024
Title: Abstracts: Systemic Sclerosis & Related Disorders – Clinical III
Session Type: Abstract Session
Session Time: 11:00AM-12:30PM
Background/Purpose: Vascular involvement is a prominent feature of systemic sclerosis (SSc). Safe and non-invasive methods to visualize cutaneous blood vessels beyond nailfold capillaries are lacking. Optical coherence tomography angiography (OCTA) is a new, non-invasive imaging modality that can provide high-quality images of vasculature; it is currently used to visualize the retinal vessels in ophthalmology. Herein, we examined this novel technology’s utility for assessing skin vessels in SSc.
Methods: All patients fulfilled the 2013 ACR/EULAR Classification Criteria for SSc. Early disease was defined as disease duration less than 3 years from non-Raynaud’s phenomenon symptom. Healthy control participants did not have an autoimmune systemic or skin disease. Predefined, standardized areas were assessed on the nailfolds, finger, hand, and forearm bilaterally. The OCTA assessors were blinded to the participants’ diagnosis. Using a swept-source OCT system built for the assessment of skin by our group, we obtained 3D OCTA images of skin. The OCT system operated at a central wavelength of 1300 nm, a scan range of 108 nm, and a scan rate of 100 kHz, with axial and lateral resolutions of 9 μm and 27.8 μm, respectively. OCTA data was acquired with 5 repeated B-scans at each B-scan position over 500 B-scans. Post-processing was done using Matlab and QuPath, employing a Hessian filter to enhance contrast and connectivity of blood vessels. Vessel lumen width, number of vessel branches, and vascular tortuosity were calculated using QuPath tools and a custom Matlab algorithm.
Results: A total of 55 SSc patients and 20 healthy controls were enrolled. The patient sample consisted of 39 individuals with a diffuse subtype (including 13 with early disease) and 16 with limited cutaneous involvement (including 6 with early disease).
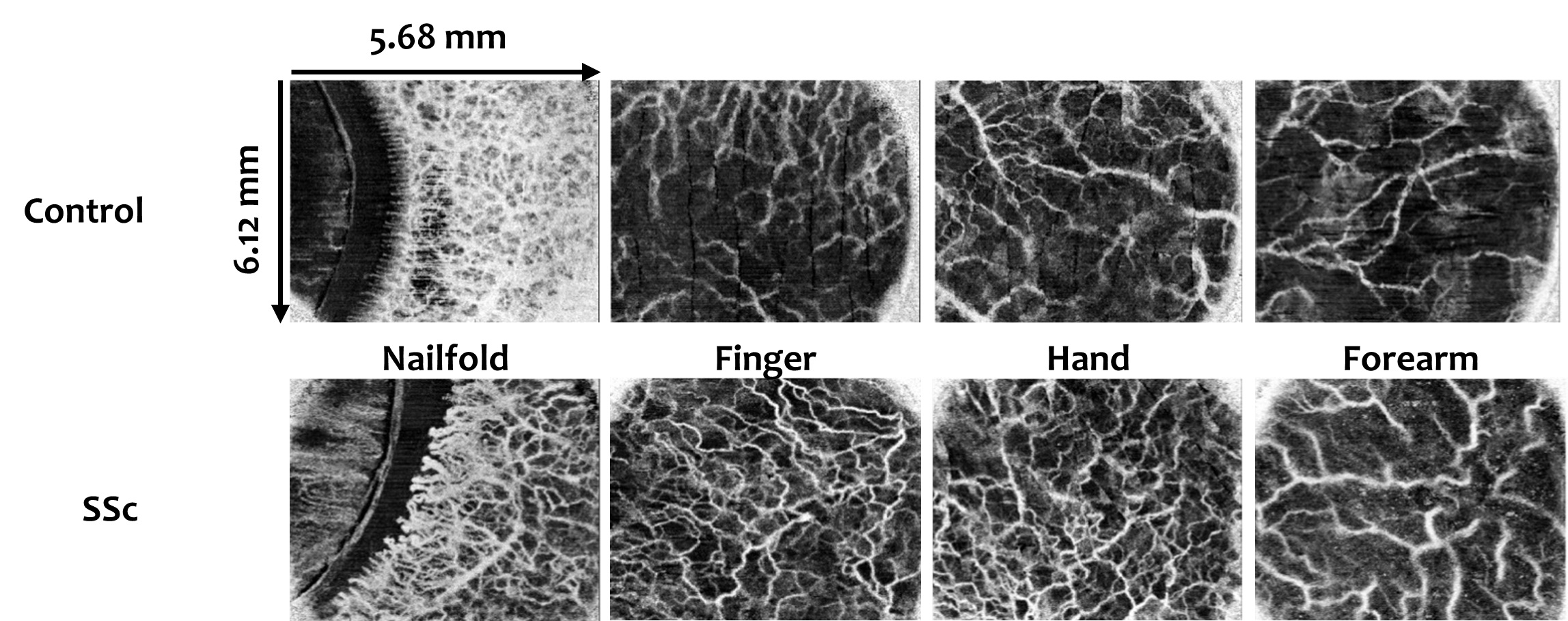
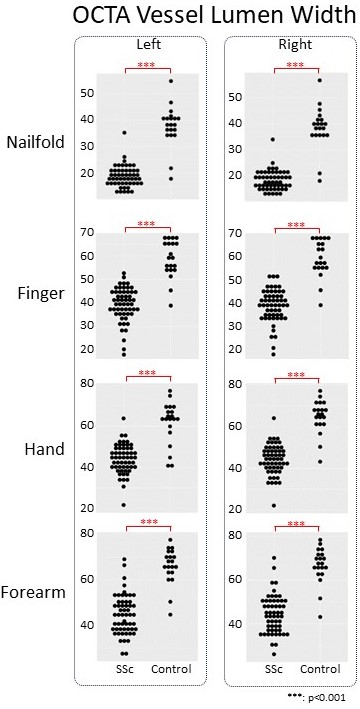
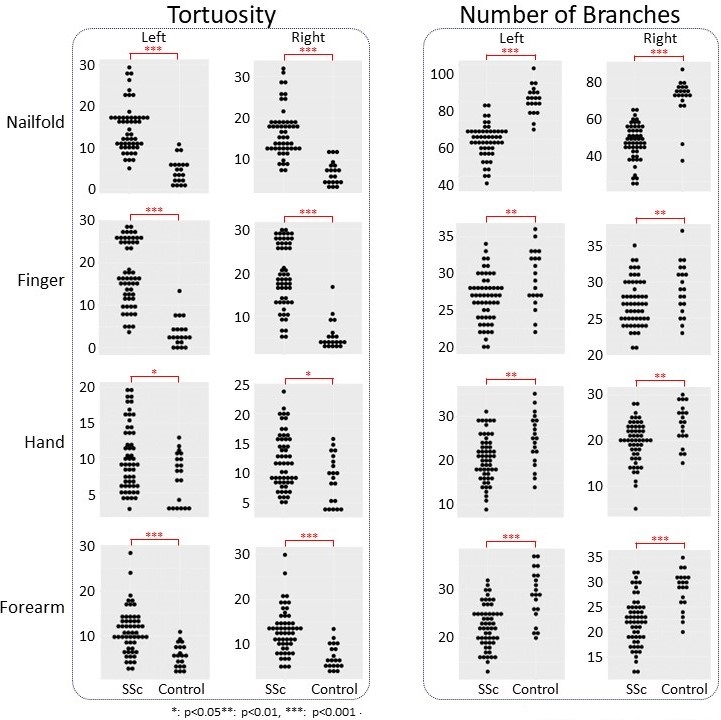
As seen in the representative images in Figure 1, OCTA was able to provide high-resolution images of cutaneous vessels in all four anatomic areas. As expected, vessel lumen width (Figure 2) and number of branches (Figure 3) were significantly lower and vascular tortuosity (Figure 3) was significantly higher in SSc patients than in healthy controls in the nailfold area. Consistent with these findings, lower vessel lumen width and number of branches, as well as higher vessel tortuosity were also observed in finger, hand, and forearm areas. The difference between SSc patients and controls was statistically significant for all comparisons. Moreover, all measurements also showed high intra- and inter-observer reliability.
Conclusion: OCTA is a safe, non-invasive method that can assess skin vascular involvement in SSc beyond nailfold capillaries. Using this novel technology, we showed that SSc patients have prominent skin vascular changes in finger, hand, and forearm areas.
To cite this abstract in AMA style:
Nikitin P, Chawla H, Singh M, Theodore S, Aglyamov S, Zhang M, Skaug B, Mayes M, Larin K, Assassi S. Optical Coherence Angiography: A Non-invasive, Safe Method for Assessing the Systemic Sclerosis Related Vasculopathy Beyond Nailfold Capillaries [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/optical-coherence-angiography-a-non-invasive-safe-method-for-assessing-the-systemic-sclerosis-related-vasculopathy-beyond-nailfold-capillaries/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/optical-coherence-angiography-a-non-invasive-safe-method-for-assessing-the-systemic-sclerosis-related-vasculopathy-beyond-nailfold-capillaries/