Session Information
Date: Monday, November 8, 2021
Title: Epidemiology & Public Health Poster III: Other Rheumatic & Musculoskeletal Diseases (1022–1060)
Session Type: Poster Session C
Session Time: 8:30AM-10:30AM
Background/Purpose: Reducing exposure to potentially inappropriate medications (PIMs) in older adults may minimize adverse drug events. The American Geriatrics Society (AGS) Beers Criteria® of Potentially Inappropriate Medication Use provides guidance regarding medications that should be avoided in older adults. Since opioids are associated with an increased risk of cognitive impairment, falls with fracture, and adverse drug-drug interactions in older adults, we also included opioids in the analysis. We used a population-based sample of older adults seen by rheumatologists to assess PIM use and identify risk factors.
Methods: Adult patients ≥ 65 years old with ≥ 2 visits in 2018 at a clinical rheumatology practice participating in the RISE registry were included. We focused on patients with 6 rheumatic diseases commonly associated with pain: OA, gout, RA, PsA, SLE, and SSc. Diagnosis was defined by ≥ 2 ICD-10 CM codes ≥ 30 days apart. Each patient was given one diagnosis for this analysis based on a simple predetermined hierarchy (OA, gout, RA, PsA, SLE, SSc). Medications of interest were those listed by the AGS Beers Criteria® with a ‘strong recommendation to avoid’, or opioids. The frequency and percent of patients with these medications listed on their medication list was determined. We developed several logistic regression models in which the outcome estimated the odds of patients taking these medications (≥1 Beers Medication, ≥2 Beers Medication, opioid, or benzodiazepine) and covariates included patient area deprivation index, age, gender, rheumatic diagnosis, Deyo-Charlson comorbidity index, insurance, and race/ethnicity. Marginal predictions and 95% confidence intervals were obtained.
Results: We included 178,833 older adults (mean age 75+/-7) from 217 practices. Forty percent of older adults seen in these rheumatology practices had a PIM on their medication list. Rates differed slightly between diseases (45% OA, 37% gout, 37% RA, 39% PsA, 42% SLE, 40% SS). Patients were most likely to have a prescription for opioids (17%), NSAIDs (12%), benzodiazepines (7%), or anticholinergics (4%). Older adults living in more socioeconomically disadvantaged neighborhoods were more likely to have an opioid prescription. Other factors associated with a higher odds of opioid prescription included female gender; OA, gout or PsA diagnosis; Medicaid insurance; and American Indian or Alaskan Natives race/ethnicity. Lower odds of opioid prescription was associated with older age and Asian race/ethnicity. Area deprivation index was not associated with other assessed PIM use (Figure).
Conclusion: Older adults with rheumatic disease were more likely to have an opioid prescription if they lived in a socioeconomically disadvantaged area. In contrast, other PIM prescriptions assessed did not vary based on the level of disadvantage in the area of residence. Future research should evaluate ways to reduce potentially harmful medications such as opioid and benzodiazepine use in older patients with rheumatic disease, and determine what factors are driving the increased opioid prescriptions associated with living in more deprived areas.
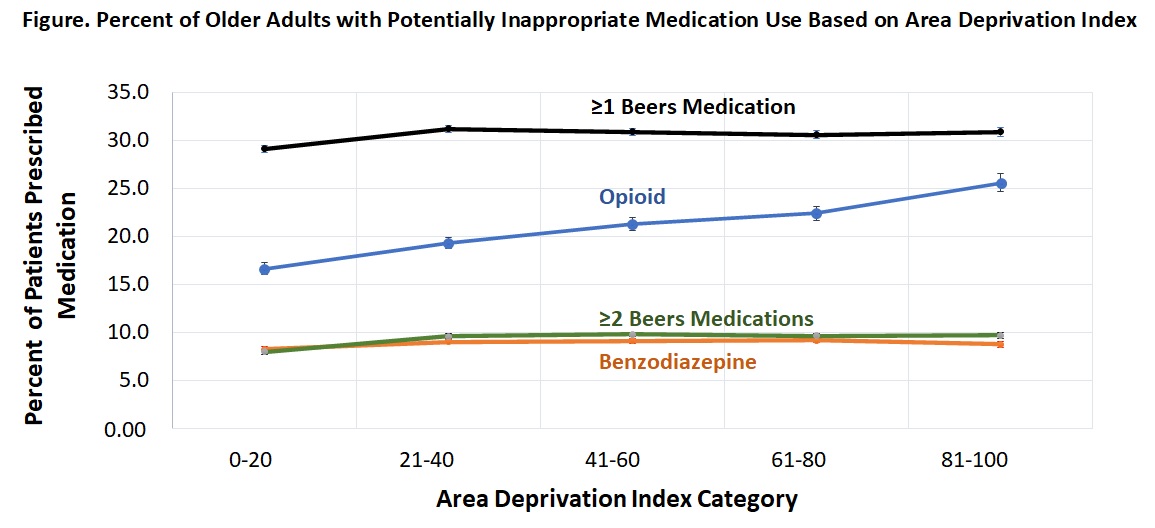 Beers Medication refers to medications listed in the American Geriatrics Society (AGS) Beers Criteria® with a strong recommendation to avoid. Marginal predictions and 95% confidence intervals from several logistic regression models with outcomes shown (≥1 Beers Medication, ≥2 Beers Medication, Opioid, or Benzodiazepine) based on patient area deprivation index and including age, gender, rheumatic diagnosis, Deyo-Charlson comorbidity index, insurance, and race/ethnicity as covariates.
Beers Medication refers to medications listed in the American Geriatrics Society (AGS) Beers Criteria® with a strong recommendation to avoid. Marginal predictions and 95% confidence intervals from several logistic regression models with outcomes shown (≥1 Beers Medication, ≥2 Beers Medication, Opioid, or Benzodiazepine) based on patient area deprivation index and including age, gender, rheumatic diagnosis, Deyo-Charlson comorbidity index, insurance, and race/ethnicity as covariates.
To cite this abstract in AMA style:
Anastasiou C, Evans M, Schmajuk G, Yazdany J. Older Patients with Rheumatic Disease Are Commonly Prescribed Potentially Inappropriate Medications [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/older-patients-with-rheumatic-disease-are-commonly-prescribed-potentially-inappropriate-medications/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/older-patients-with-rheumatic-disease-are-commonly-prescribed-potentially-inappropriate-medications/
