Session Information
Session Type: Abstract Session
Session Time: 4:30PM-5:30PM
Background/Purpose: Obesity has been linked to chronic pain and pain sensitization in the general population and among patients with rheumatoid arthritis (RA). The mechanism by which obesity leads to pain sensitization remains unclear. Adipocytokines, including adiponectin, leptin, and Fibroblast Growth Factor-21, are metabolic regulators that are highly associated with obesity and inflammation and may serve many biologic functions surrounding energy utilization. Associations between adipokines and chronic pain has been observed in other settings. We aimed to determine whether adipocytokines are associated with pain, polysymptomatic distress, and trajectories of pain in patients with RA over time in a large patient registry.
Methods: The study was conducted in a subset of Forward; a patient-based multi-disease, multi-purpose rheumatic disease registry with patients enrolled from community-based rheumatology practices across the United States.. Adipocytokines were measured on stored serum. Body mass index (BMI), pain on visual analogue scale (VAS), polysymptomatic distress, and other patient-reported outcomes (PROs) were reported on bi-annual questionnaires. Linear regression was used to evaluate independent associations between obesity, adipocytokines, and PROs at the time of laboratory assessment. Cox proportional hazards models were used to evaluate independent associations between adipocytokines (leptin, adiponectin, fibroblast growth factor [FGF]-21) and clinically meaningful changes in pain over time – defined as a change of more than 1.1 in visual analogue scale (VAS) sustained over two surveys. These models were adjusted for demographics, baseline pain, BMI, C-Reactive Protein levels, anti-citrullinated protein autoantibodies (ACPA) status, the rheumatic disease comorbidity index (RDCI), osteoarthritis, depression, and diabetes.
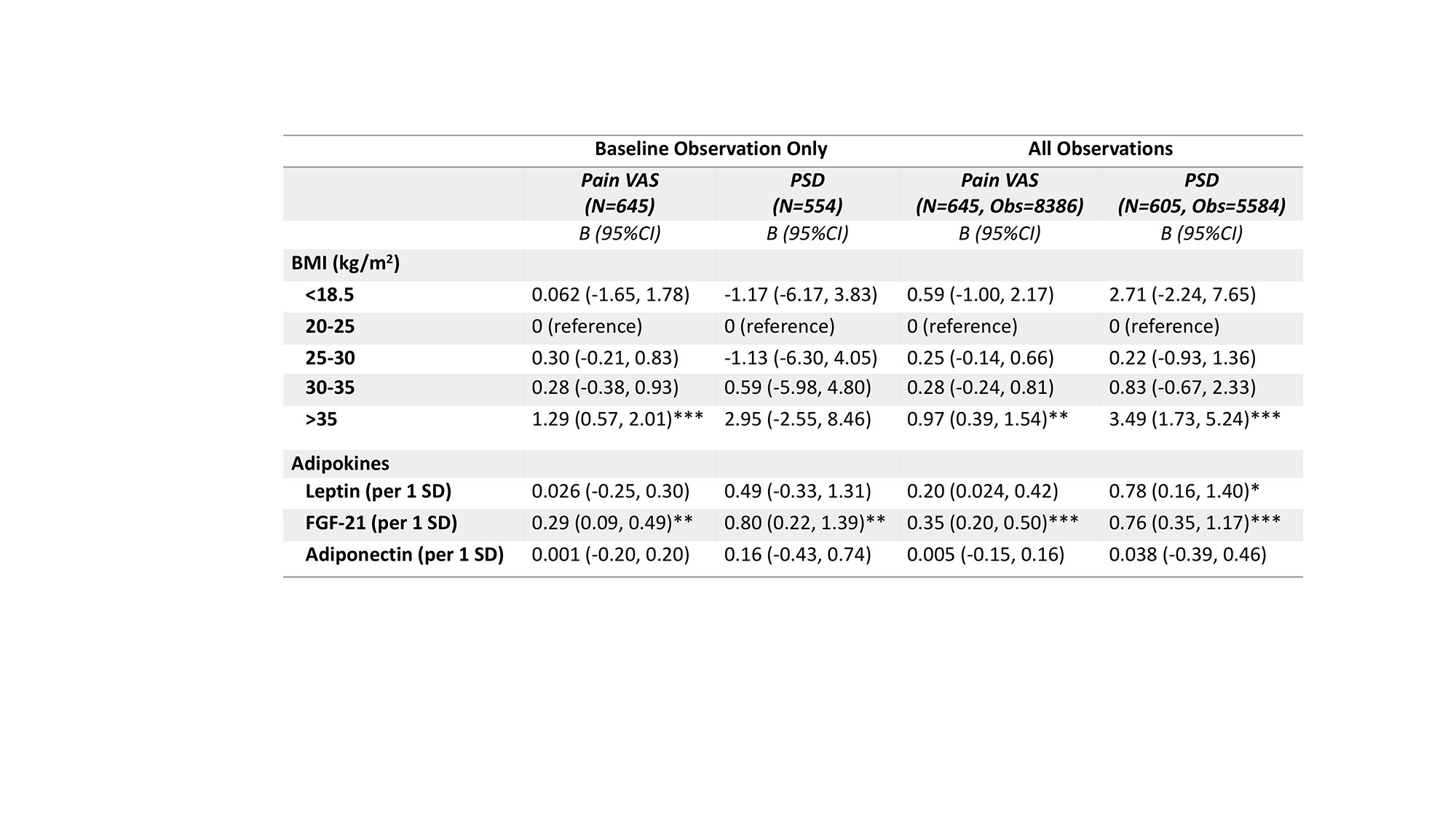
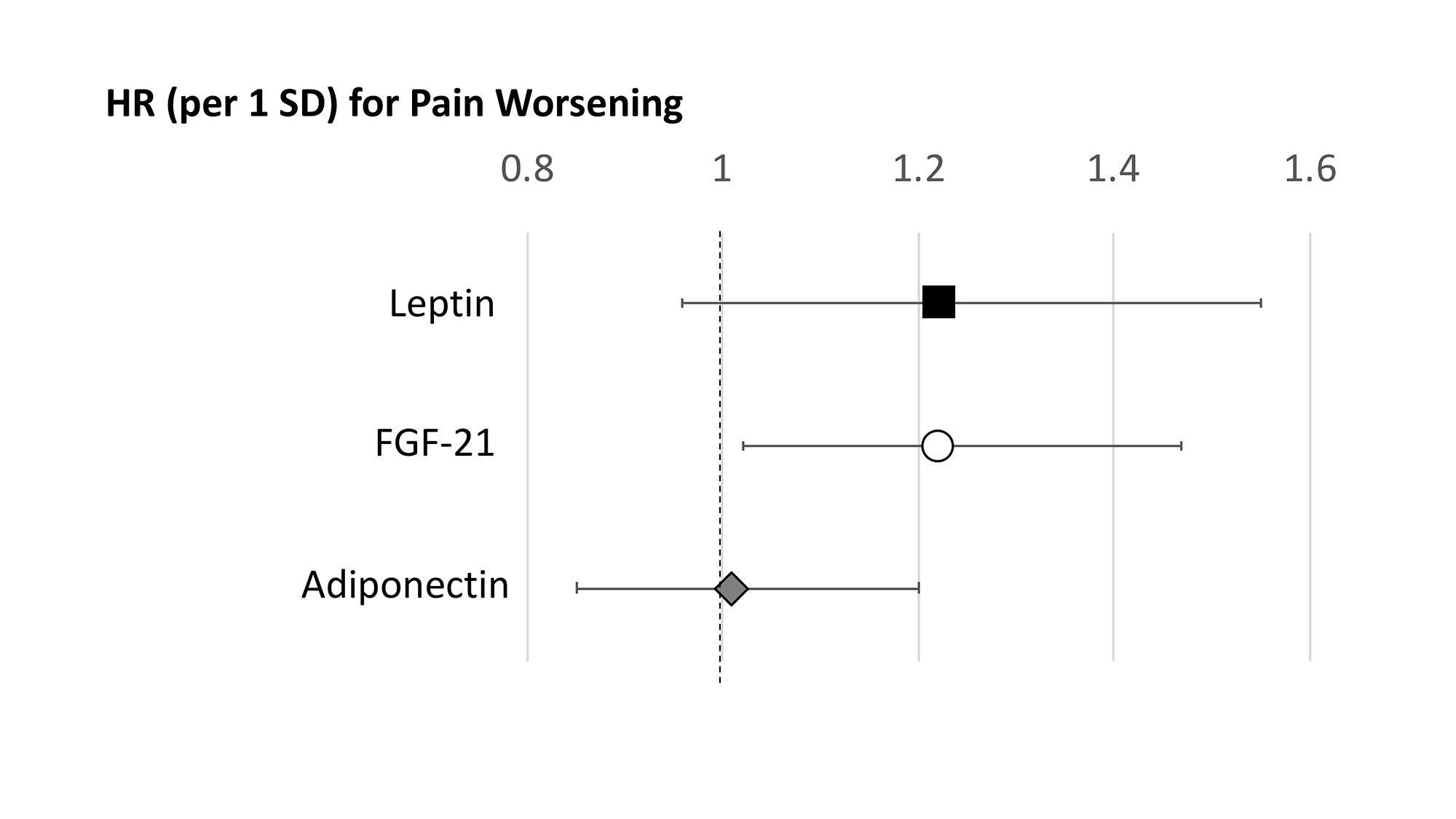
Results: Among 645 patients included in these analyses, there were significant differences in RA characteristics, comorbidity, PROs, and adipokines across obesity categories (Table 1). Of note, severely obese patients were more likely to experience greater pain on VAS and greater polysymptomatic distress. Higher FGF-21 levels were independently associated with greater pain and greater polysymptomatic distress at baseline and over subsequent observations (Table 1), as well as a higher probability of taking opioids [OR per 1 SD: 1.50 (1.21, 1.85) p< 0.001] at baseline. Higher FGF-21 levels were also associated with higher likelihood of worsening pain over time (Figure 1), and a nonsignificant decrease in the likelihood of improving [HR (per 1 SD): 0.87 (0.73, 1.03) p=0.10].
Conclusion: Severe obesity and elevated levels of FGF-21 are each independently associated with pain, polysymptomatic distress, and opioid use in RA. Elevated FGF-21 levels may help identify those at risk of worsening pain trajectories. Mechanistic studies are needed to determine if adipocytokines could serve as targets for interventions.
*p=0.05; **p<0.01; ***p<0.001
To cite this abstract in AMA style:
Baker J, Wipfler K, Olave M, Pedro S, Katz P, Michaud K. Obesity, Adipokines, and Chronic and Persistent Pain in Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/obesity-adipokines-and-chronic-and-persistent-pain-in-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/obesity-adipokines-and-chronic-and-persistent-pain-in-rheumatoid-arthritis/